Master’s Thesis by Anett Hörster
A Comparison of Osteopathy with Manual Therapy (according to the CRAFTA® Concept) in the Treatment of Patients with Craniomandibular Dysfunction. A Clinical Pilot Study.
Master’s Thesis submitted in fulfillment of the requirements for the degree of Master of Science in Osteopathy
Danube University Krems, submitted at the Vienna School of Osteopathy. November 2008. Anett Hörster.
Topic: Comparison of osteopathy with manual therapy (according to the CRAFTA® concept) for the treatment of patients with craniomandibular dysfunctions
(CMD). Methodology:
- Study design: Randomized controlled trial (RCT) / Clinical pilot study
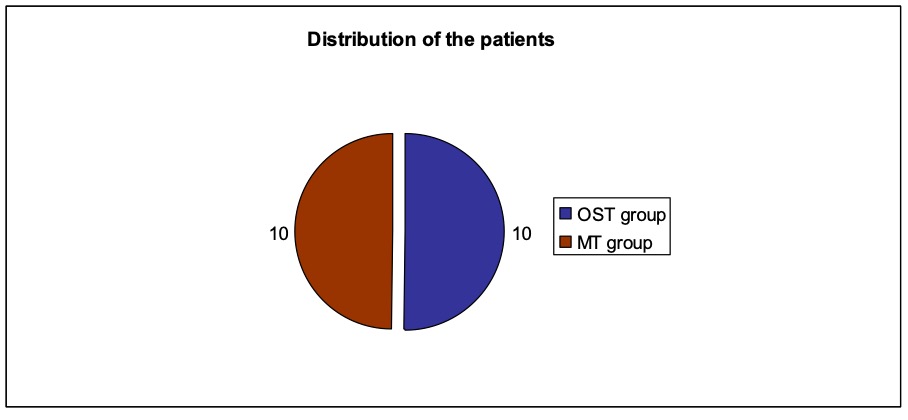
- Patients: 20 participants (18 female and 2 male) aged between 19 and 65 years. The patients were randomly divided into two groups. The result was a distribution of 10 patients (9 female and 1 male) in the study group osteopathy and 10 patients (9 female and 1 male) in the comparison group manual therapy (according to the CRAFTA® concept).
- Measurement parameters (and measuring methods): Pain (VAS assessment and SES questionnaire), health-related quality of life (SF36 questionnaire), mouth opening (inter-incisor distance (IID) measurement), muscle tension (Biofeedback EMG measurement).
- Inclusion criteria: Pain in the region of the muscles of mastication, bruxism (grinding) or bracing (compressing), deviation when opening the mouth, restricted ability to open the mouth, clicking noise when opening the mouth.
- Exclusion criteria: Pronounced dysgnathia, facial pain due to systemic, neurological or psychiatric diseases, acute or chronic TMJ trauma, sinusitis.
- Treatment procedure: Three treatments per patient within a period of two weeks following a black-box approach. The measurements and interrogations were carried out before the first and after the last treatment. The patients in the study group osteopathy were treated by the author Anett Hörster, the patients of the comparison group by a certified CRAFTA® therapist.
Results: Regarding the measurement parameters pain, mouth opening and muscle tension both, osteopathy and manual therapy (according to the CRAFTA® concept) facilitate significant improvements for the treatment of patients with CMD. In this context osteopathy is significantly more effective concerning the parameter pain. Regarding the health-related quality of life only osteopathy has a significant effect and in comparison works significantly better than manual therapy (according to the CRAFTA® concept) which could not achieve an improvement of this parameter at all. Key words: Craniomandibular dysfunction (CMD), osteopathy, manual therapy (according to the CRAFTA® concept).
Today more and more patients suffer from chronic headaches, facial, neck or back pain (cf. Kares et al. 2001). Also problems like tinnitus, bruxism and disturbed mobility of the temporomandibular joint (TMJ) occur in increasing numbers in today’s performance-oriented society (cf. Köneke 2005).
Patients who have these kinds of pain or restrictions are often sent from one doctor or therapist to the next one because the description of their problems makes it difficult to apply a systematic and precise diagnostic method and thus find an effective therapy. Quite often the patients therefore have to go though a long process of suffering (cf. Plato 2001).
Many times the reason for this can be found in the complex and multi-causal interrelations and diversity of symptoms of the clinical picture of craniomandibular dysfunctions (CMD). Due to the lack of a clear leading symptom and the fact that various etiologic factors might have a different significance in each individual case, is it difficult to comprehend and classify CMD with its multi-faceted symptoms
(cf. Ahlers et al. 2007).
There are many different possibilities of treating CMD, e.g. pharmacological therapy, correction of occlusion, orthodontics, acupuncture, surgical interventions, psychotherapy and speech therapy as well as various ways of manual therapy and physical therapy (cf. Hippel 2006, Kehr 2005). A survey in this context showed that about 80 percent of all patients with CMD symptoms were treated most effectively with conservative treatment methods (cf. Dimitroulis et al.1995).
Due to the described problems is the development of an interdisciplinary approach of diagnosis and therapy a great challenge for dentists, orthopaedists, osteopaths and physical therapists to offer patients, in particular the ones with chronic pain and restrictions, possibilities of early intervention to regain their health and quality of life (cf. Türp 2002, Dapprich 2007).
As osteopath and certified CRAFTA® therapist the author has been concerned with CMD for several years and is treating patients with the above mentioned symptoms every day in her practice. Due to the question of a physician: “What am I supposed to write on the prescription: Manual therapy or osteopathy – what has the better effect?” the idea for this thesis was born, especially since the relevant medical literature could not answer this question.
Figure 1 shows the most common treatment possibilities for patients with CMD
(cf. Hippel 2006, Kehr 2005). It also represents the conceptual framework of this thesis. Six relevant papers and studies pertaining to the possibilities of manual and physical therapy could be found in the research process. They are numbered consecutively and described briefly in the following section. Figure 1 shows to which treatment category these papers and studies belong. The red circle with the question mark indicates the question dealt with in this thesis.
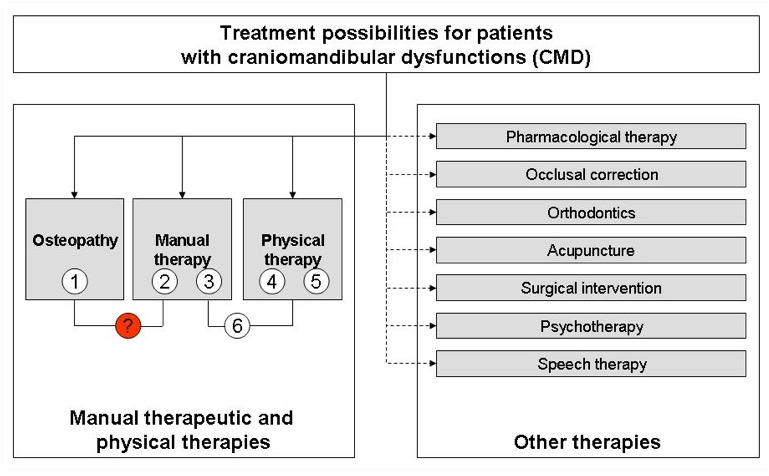
Figure 1: Conceptual framework of the thesis
- A pilot study by Butenschön and Mitha (2002) could prove the influence of osteopathic treatment with a so-called “four hand contact” on CMD. The occlusal index (according to Slavicek) showed a significant improvement. However, the analysis of the mandibula position indicator (MPI) did not provide a significant result.
- A CRAFTA® pilot study showed by using a questionnaire that (mainly manual-therapeutic) neuromusculoskeletal treatments by certified CRAFTA® therapists could clearly improve the craniomandibular and craniofascial dysfunctions
(cf. von Piekartz 2007). - In a randomized clinical pilot study Demling et al. (2008) compared the treatment of CMD with a Michigan splint with the treatment of a Michigan splint in combination with physical therapy (following the guidelines of manual therapy). In both groups a significant reduction of the overall pain, pain during rest and under strain could be observed as well as a significant improvement of the inter-incisor distance (IID). The comparison of the two groups showed that the difference was only significant regarding the active IID (significant improvement due to the combined treatment of a Michigan splint with physical therapy).
- Nicolakis et al. (2001) examined the effectiveness of physical therapy treatments including massage, stretching, isometric contraction exercises, guided mouth opening and closing movements, manual traction on the jaw, posture training and relaxation techniques. Significant improvements of pain, discomfort and mouth opening could be noticed.
- A study which was carried out at the University of Cologne under the direction of Prof. Kerschbaum (2001) over a period of several years confirmed the effect of physical therapy. More than 100 patients with myoarthropathies reported an average pain reduction of 30 % on the VAS.
- A comparison of manual therapy and exercise therapy for craniomandibular dysfunctions was carried out by Knust (2006) in a pilot study. Both treatment methods showed significant improvements of the subjective pain perception, mouth opening and pain-on-pressure points in the muscles, with the pain perception clearly improving through manual therapy. The conclusion of this study by Knust is that both treatment options are effective with regard to CMD and should be used side by side to achieve the best possible synergy effects.
Considering the results of the literature research the first thing to be noticed is that only very few papers and studies evaluate the effectiveness of manual and physical therapeutic treatments for CMD. Only two studies provide some results for the physical therapy and two others regarding manual therapy. Although these studies indicate some significant improvements, they were only pilot studies and in part applied only one measurement method. So far there is only one pilot study looking at the effectiveness of osteopathy. But in this particular study an extraordinary treatment approach involving two therapists (four hand contact) was chosen. There is also only one pilot study to date comparing manual with physical therapy in the case of CMD.
Overall there seems to be a lack of information regarding the effectiveness of manual and physical therapy forms in the case of CMD, which holds in particular true for osteopathy and the comparison of the various therapy forms with each other.
1.1 Objective of the thesis
This thesis shall close the existing information gap regarding the effectiveness of various forms of manual and physical therapy for patients with craniomandibular dysfunctions. To achieve this objective osteopathy is compared with manual therapy (according to the CRAFTA® concept) in a clinical pilot study treating patients with CMD.
1.2 Hypothesis
Osteopathy shows better results in the treatment of patients with craniomandibular dysfunctions than manual therapy (according to the CRAFTA® concept).
1.3 Structure of the thesis
Chapter 2 provides the theoretical background for this thesis. For this Chapter 2.1 presents the underlying anatomical information around the stomatognathic system with focus on the temporomandibular joint (TMJ). The subsequent chapter 2.2 explains the manual therapy according to the CRAFTA® concept while Chapter 2.3 describes osteopathy. Finally, Chapter 2.4 explains the craniomandibular dysfunction, points out functional interrelations and gives an overview of possible forms of therapy with the focus on a comparison of osteopathy with manual therapy.
Chapter 3 presents the chosen methodology and the design of this clinical pilot study. For this Chapter 3.1 describes how the participants were recruited, which inclusion and exclusion criteria were applied and how the test persons were randomly divided into the study and comparison group. The examination and treatment procedures are described in Chapter 3.2. The measurement parameters and methods that were applied are explained in Chapter 3.3. Finally, Chapter 3.4 provides explanations regarding the statistical analysis of the collected data.
Chapter 4 presents the results of the study for the different measurement parameters, which are then finally discussed in Chapter 5.rden.
2.1 Anatomical structures
The following sub-chapters explain the underlying anatomical background necessary to understand CMD and its complexity. The focus lies on the temporomandibular joint (TMJ) which plays a central role in CMD. Chapter 2.1.1 presents first of all the stomatognathic system and its related structures with the TMJ as its centre. Chapter 2.1.2 presents the embryology and describes how the TMJ and its related structures develop. Chapters 2.1.3 to 2.1.5 provide a short overview of the most important anatomical structures around the TMJ.
2.1.1 The stomatognathic system
The stomatognathic system (mouth-jaw-system) is a complex system of interrelated elements and not a single seizable morphological organ. It is a physiological unit and its main functions are eating, speaking and breathing, which also include the aspects body posture and stress management (cf. Amigues 2005).
Local disturbances in this system can lead to dysfunctions and pain in more distant regions (cf. Gernet et al. 2000). Chapter 2.4.4 takes a closer look on the functional connections.
Figure 2 is a simplified diagram of the stomatognathic system with its fundamental structures. It illustrates in particular how much the TMJ is involved in the vertical statics of the body.
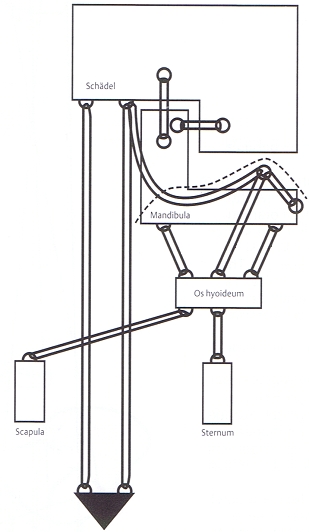
Figure 2: Model of the TMJ integration
in the vertical body statics, Liem, 2000, page 288
The individual structures that form the stomatognathic system are the following
(cf. Siebert 2000, Milne 1999):
Bones:
- Os occipitale (1 bone)
- Os temporalia (2 bones)
- Os sphenoidale (1 bone)
- Os maxillae (2 bones)
- Mandible (1 bone)
- Hyoid (1 bone)
- Os claviculae (2 bones)
- Os scapulae (2 bones)
- Sternum (1 bone)
- Os costae 1 and 2 (4 bones)
- Os vertebrae C1 to D 3 (10 bones)
Joints:
- Art. temporomandibularis (TMJ)
- Art. atlantooccipitalis, -axiales (O/A joint)
- Art. sternoclavicularis (sternoclavicular joint)
- Cranial sutures
Muscles:
Fusiform, flat, double-feathered and multi-bellied
forms; the most important ones are:
- uprahyoidal and infrahyoidal muscles
- M. pterygoideus laterales et mediales
- M. masseter
- M. temporalis
- M. digastricus
- M. omohoyideus
Fascia:
- superficialis
- cervicalis
- praevertebralis
- infrahyoidea
- praetrachealis
- the fascia of the M. temporalis, M. masseter, M. trapezius, sternocleidomastoideus and M. pectoralis major
- Aponeurosis epicranialis (tendinous sheet that covers the cranial vault)
Teeth:
- dental enamel
- cement
- dentine
The head of a four-week old human embryo consists mainly of the brain which is covered by thin membranes of mesodermal and ectodermal origin (cf. Sadler 1998). In the fourth week the pharyngeal arches, which play an important role in the development of the head and neck, start to develop. The upper and lower jaw with the muscles of mastication develop from the first pharyngeal arch, while the hyoid bone, which later fuses with the heart bulge, develops from the second pharyngeal arch (cf. O’Rahilly et al. 1999).
During the seventh week of embryologic development the articulation between malleus and incus form at the dorsal end of Meckel’s cartilage. It is a phylogenetic primary joint and for a short time acts as jaw joint, i.e. opening of the mouth is possible.
Once the space of the middle ear develops this primary joint looses its connection with the mandible. Due to the contact of the mandible with the temporal bone the secondary jaw joint is formed, which can be seen in Figure 3. From the 26th week onwards a completely developed TMJ with the physiological upper and lower joint margins can be recognized (cf. Bumann et al. 2000, Rauber et al. 1987).
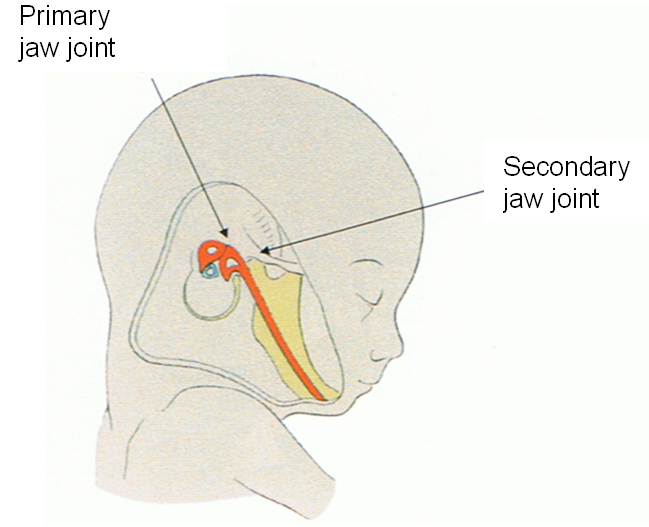
Figure 3: The primary jaw joint is replaced by the Articulatio temporomandibularis
as a secondary jaw joint, Breul, 2005, page 17
The temporomandibular joint is formed by the mandible (lower jaw) and the Os temporale (temporal bone). The Os temporale plays the key role in the TMJ
(cf. Magoun 1974) due to the great number of structures that surround and influence this bone. The most important structures that are related to the temporal bone are (cf. Lang 2001):
- Tentorium cerebelli (tent of the cerebellum)
- cranial nerves: N. oculomotorius, N. trochlearis, N. trigeminus, N. abducens, N. facialis, N. vestibulocochlearis, N. glossopharyngeus, N. vagus, N. accessorius
- M. sternocleidomastoideus
- M. temporalis
The parts of the temporal bone that contribute to the TMJ are the anterior part of the Fossa mandibularis and the Tuberculum articulare. The part of the mandible that articulates with the temporal bone is the Caput mandibulae, the head of the mandible. The TMJ is a synovial joint consisting of an upper disco-temporal gliding joint and a lower disco-mandibular hinge joint. The Discus articularis (articular disc) of the TMJ is a transversal oval platelet made up of tight collagen-fibrous connective tissue and fibrous cartilage. The disc is anteriorly, medially and laterally fused with the joint capsule and separates the joint cavity in two chambers. In the anterior compartment the disc has contact to the M. pterygoideus laterales. The TMJ is surrounded by a loose joint capsule which runs funnel-shaped from the Os temporale to the Caput mandibulae. The most important ligaments that fortify the joint capsule and/or contribute to the movements of the jaw are the following (cf. Bumann et al. 2000, Rauber et al. 1987):
- Lig. temporomandibulare
- Lig. stylomandibulare
- Lig. sphenomandibulare
Muscles of various functions and origins play a role in the act of mastication. They have already been listed in the description of the stomatognathic system in Chapter 2.1.1. The muscles of mastication in a narrower sense are the M. masseter, M. temporalis, M. pterygoideus laterales and mediales which are located in the region of the face. The M. masseter is the strongest muscle for closing the jaw. The function of the M. temporalis is to close the jaw, retrusion, laterotrusion and the stabilization of the TMJ during non-mastication and mastication movements. The M. pterygoideus lateralis contributes to the initial opening of the mouth as well as protrusion and laterotrusion of the lower jaw. The function of the M. pterygoideus medialis is to lift and laterally deviate the lower jaw. Also responsible for opening the mouth are both the superior hyoid muscles with the M. digastricus, M. stylohyoideus, M. mylohyoideus and M. geniohyoideus and the inferior hyoid muscles to fix the hyoid bone (cf. Ahlers et al. 2007, Rauber et al. 1987).
Vascularization and innervation
The arterial blood supply of the TMJ and the muscles of mastication is mainly guaranteed via the A. temporalis and A. maxillaris. The condyle is supplied by the arterial network of the A. alveolaris inferior. The venous drainage is effected via the V. temporalis superficialis and the Plexus maxillaris and pterygoideus. (cf. Bumann
et al. 2000).
The masticatory apparatus is innervated by the third branch of the trigeminal nerve. The N. trigeminus is the only cranial nerve which has a connection to all other cranial nerves (in particular VII, VIII, XI and XII) in the region of its nuclei. With its nuclei in the brainstem (Ncl. spinalis oralis et interpolaris) it approaches the nuclei of the three most superior spinal nerves. This represents a direct link (in the sense of a so-called convergence) between the craniomandibular system and the upper cervical spine via multi-receptive neurons in the Medulla oblongata. On an efferent level the
N. mandibularis supplies the muscles of mastication. This motor efference is closely interlinked with the cervical segments C1 – C3. The sympathetic innervation is effected by the Ganglion cervicale superius (cf. Bumann et al. 2000, von Heymann 2007).
Manual therapy according to the CRAFTA® concept
The origin of manual treatment dates back to times long before medicine (as it is known today) existed. Old Chinese, Persian and Indian scriptures already allude to manual treatment techniques, which later on were taken on by the founders of modern medicine like Hippocrates, Galen and others, who also described them in their books (cf. van den Berg et al. 2002). Translated literally “manual therapy” means “healing treatment with the hands”. Nowadays modern manual therapy stands for a systematic physiotherapeutic examination and treatment of the locomotor system. Commonly manual therapy can be differentiated into four techniques
(cf. Dahl et al. 1999):
- Traction
- Translation
- Mobilisation
- Manipulation
Manual therapy according to the CRAFTA® concept is a special therapy concept which focuses in particular on complaints of the throat, neck, head and face regions and their treatment. The concept is based on an interdisciplinary approach of diagnosis and treatment. In addition to the general treatment techniques (cf. above)
a therapy according to the CRAFTA® concept also applies the following techniques (cf. von Pickartz 2005):
- Compression
- Muscular soft tissue treatment
- Neurodynamic mobilisation
On the basis of a thorough case history the problem of the patient is meticulously analyzed. The next step is a thorough functional evaluation, focusing mainly on the TMJ, the head and the related muscles and nerves. If necessary also other regions like the spine, shoulder girdle and hips are considered later on.
The treatment consists of manual therapeutic techniques for the head, neck and face on the one hand and an accompanying program on the other hand. How this accompanying program is designed usually depends on the behaviour of the patient in everyday life. It comprises various strategies of pain management. The training with the patient usually is aimed at changing specific ways of behaviour in everyday life that could cause problems (cf. von Pickartz 2005).
Figure 4 presents a schematic diagram of the above described procedure.
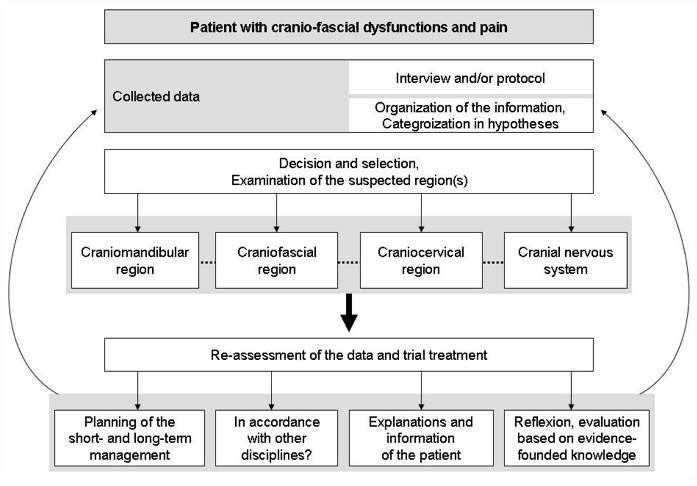
Figure 4: Overview “Patient with cranio-fascial dysfunctions and pain”,
von Piekartz, 2005, page 20
Osteopathy is an independent holistic form of medicine which grasps the human being with all the multi-layered structural, functional and biochemical interrelations.
In osteopathy the body is divided into three related anatomical systems: the parietal, visceral and craniosacral system. These are in a dynamic balance and are always regarded and treated as mutually influencing each other (cf. Croibier 2006).
In his book “Philosophy of Osteopathy” Still (1899) described the cornerstones on which osteopathy is based.
- The human being is a unit.
- Structure governs function and function forms the structure.
- The self-healing powers of the body.
An osteopathic diagnosis is based on two fundamental elements: the case history and the clinical examination. In contrast to the manual therapy (according to the CRAFTA® concept) an osteopathic examination first looks at the whole body to gain an impression of the overall picture. How the examination continues depends on the first findings. The aim is to establish a differential diagnosis.
The principles of an osteopathic diagnosis are (cf. Croibier 2006):
- An osteopathic diagnosis evaluates the quantitative and qualitative aspects of the body’s mechanics.
- An osteopathic diagnosis does not exclusively focus on the spine and joints.
- An osteopathic diagnosis evaluates the relationship structure – function.
- An osteopathic diagnosis is holistic and respects the idea of the human being as a unit.
- An osteopathic diagnosis tries to differentiate between cause and effect.
- An osteopathic diagnosis is always related to the individual.
The osteopathic therapy depends on the actual findings, i.e. the treatment focuses on the so-called dysfunctions that have been identified as causes in the examination. The result is an individual treatment approach for every patient, that can comprise parietal, visceral and/or craniosacral techniques (cf. Hippel 2006).
With regard to TMJ problems one can differentiate between the treatment of ascending and descending dysfunctions. Ascending dysfunctions are disturbances of the function or in the tissues below the head and neck (thoracic outlet), which can affect the TMJ, e.g. dysfunctions in the foot, oblique pelvis position or visceral disturbances (cf. Liem 2000). If such ascending parietal, visceral or craniosacral dysfunctions are found to have an influence on the TMJ and its surrounding structures, these are considered before the actual treatment of the craniomandibular system (cf. Hippel 2006).
Descending dysfunctions are disturbances directly in the region of the head, jaw and neck/throat, e.g. disturbed occlusion or misaligned C1 joint, which could provoke disturbances in the tissues or of the function in other body structures. These descending dysfunctions are treated directly within the craniomandibular and craniocervical areas.
The English term “craniomandibular disorders” (cf. McNeill 1990) was adopted by the German Society for dental, oral and craniomandibular therapies (Deutschen Gesellschaft für Zahn-, Mund- und Kieferheilkunde, DGZMK) and the German Society for function diagnostics and therapy (Deutschen Gesellschaft für Funktionsdiagnostik und –therapie, DGFDT) as “craniomandibular dysfunctions” with the international abbreviation “CMD” (cf. Ahlers et al 2007). The clinical picture of CMD summarizes all painful and painless conditions which can be ascribed to structural, functional, biochemical and psychological dysregulations of the function of muscles and/or the TMJ (cf. Köneke 2005).
Disturbed functions of the craniomandibular system can have many different reasons and are expressed through various signs and symptoms in the muscles of mastication, the TMJ or the locomotor system (cf. Slavicek 2004). Already in 1934 Costen described a syndrome that linked facial pain, symptoms of the ear and functional disturbances of the stomatognathic system. Chapter 2.4.4 will take a closer look on the functional interrelations.
Today CMD is considered and treated in different ways by different medical specialities, which is also reflected by the different nomenclatures that are used
(cf. Ahlers et al. 2007, von Pickartz 2005). Following the DGZMK definition, the abbreviation CMD is used in this paper for any disturbance of function of the craniomandibular system.
In the following Chapter 2.4.1 the aetiology and symptoms of CMD are discussed, while Chapter 2.4.2 presents its epidemiology. The summary of the various classifications in Chapter 2.4.3 reflects only the most common models and those that are relevant in the context of this paper. Since there are important functional interrelations between the TMJ and the rest of the body’s support system, Chapter 2.4.4 looks in particular at the statics of the neck and shoulder girdle as well as their connections with the stomatognathic system. Finally, Chapter 2.4.5 compares the two treatment concepts applied in this paper: osteopathy and manual therapy according to the CRAFTA ® concept.
In 2004 Ververs et al. carried out a literature research regarding the aetiology of CMD. They found 116 publications on the topic and concluded that “even though the multi-factorial aetiology of craniomandibular dysfunctions (CMD) is widely accepted, scientific evidence is lacking” (Ververs et al. 2004, 556). On the basis of this literature research Ververs et al. classified the aetiological causes of CMD in three main groups: the first group comprises occlusal-anatomical factors like occlusal interferences or missing teeth in the distal supporting zone. The second group includes neuromuscular factors like parafunctions and habits. The third group considers psychosocial factors like certain personality traits, stress, traumatic events (divorce, unemployment, death of relatives) and cultural aspects. These three groups can influence each other. To what extent the factors of the three groups have an effect on the individual patient can vary. Therefore different symptom profiles can develop.
Also systemic diseases can be the cause or promoting factor for the development of CMD. They can be of degenerative, endocrine, infectious, metabolic, neurological or vascular nature (cf. McNeill 1990).
Honikel (2007) expands this model from an osteopathic perspective and adds arthrogenic, craniogenic, viscero-fascial and vertebrogenic causes, which generates a comprehensive spectrum of possible causes. This extended model by Honikel is used in this paper. All possible causes with examples are summarized in the list below:
Arthrogenic:
- Luxation or subluxation of the articular disc
- Degenerative, inflammatory changes
- Trauma etc.
Dento-occlusogenic:
- Disturbances of the static and dynamic occlusion
- Loss of teeth
- Bite anomalies (cross-bite) etc.
Neuro-myogenic:
- Disturbances of cranial nerves
- Neuromuscular dysbalances etc.
Psychogenic:
- Stress
- Depression etc.
Postural-vertebrogenic:
- Dysfunctions of C0/1, C1/2, C2/3
- Disturbances in the arches of the foot etc.
Craniogenic
- Dysfunctions and lesions of the bones that directly or indirectly contribute to the TMJ
Viscero-fascial:
- Irritation of the diaphragms
- Disturbances of the respiratory tract
Other:
- Impairment of breathing (open bite, chronic sinusitis)
- Excessive chewing of chewing gum
- Prone position etc.
- Systemic diseases
The symptoms of CMD are multi-facetted as illustrated in Figure 5 which focuses on the head only.
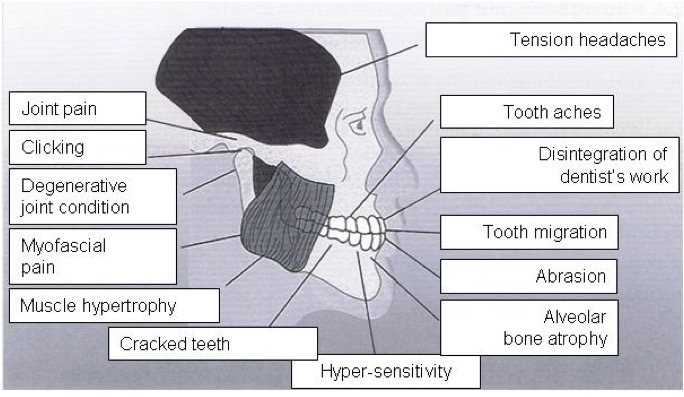
Figure 5: Symptoms of a CMD, Ahlers et al., 2007, page 92
Looking at the whole body, the CMD symptoms can be categorized in arthro-dentogenic, postural and indirect symptoms (cf. Honikel 2007):
Arthro-dentogenic
- Tooth ache without structural correlate
- Abrasions in the affected dental region
- Restricted opening of the mouth
- Crepitation during movements of the TMJ
- Clicking sounds etc.
Postural:
- Morning headaches or neck pain
- Restricted mobility of the hyoid
- Oblique pelvis position
- Static foot complaints
- Myofascial dysfunctions etc.
Indirect
- Tinnitus
- Dizziness/vertigo
- Diffuse fascial pain
- Problems with swallowing or phonation
- Ophtalmological problems etc.
Epidemiologic evaluations have shown that 44 – 75% of the world population have clinical signs of CMD, with 20 – 33 % displaying clinical symptoms, but only 3 – 4% contacting a therapist (cf. De Knater 1993). In Germany the incidence of CMD symptoms among the adult population ranges only around 10% (cf. Gesch et al. 2004).
Women are more frequently and heavily affected than men. One reason for the prevalence of the problem among women could be the hormonal balance, in particular the metabolism of oestrogen (cf. Le Resch et al. 2003). Already in 1997 Le Resch found out that the intake of oral contraceptives had the consequence that female CMD patients experienced less pain-free days.
Numerous models of CMD classifications are available. They apply different diagnostic criteria and clinical pictures. This great number can be ascribed to the lack of agreement regarding the aetiological factors and their interaction (cf. von Piekartz 2005). The following section will briefly present the three most important classification models.
For example, the American Academy of Orofacial Pain (AAOP) classifies CMD diagnosis-specific in arthropathies and myopathies. The dysfunctions of the TMJ are further divided into large sub-groups. In this classification is also the range of primary TMJ diseases included. However, clear inclusion or exclusion criteria are not provided (cf. Ahlers et al. 2007).
The International Headache Society (IHS) uses a classification on 13 different levels, which provides a basis to establish a diagnosis (cf. Piekartz 2005, Ahlers et al. 2007). This classification system is hardly used in practice by dentists, physical therapists or osteopaths because it focuses mainly on headaches.
Another model was developed by Dworkin and LeResche in 1992. This classification system (Research Diagnostic Criteria) uses two axes:
On the first axis (physical parameters) three groups are differentiated. The first group includes myogenic dysfunctions. The second group comprises the range of misalignments and deviations of the articular disc. The third group is composed of arthrotic and arthralgic dysfunctions. Only one of the myogenic dysfunctions of the first group can apply to one patient, while each TMJ can in addition have an arthrogenic dysfunction of the second group and/or third group.
The second axis includes pain-related psychosocial factors and non-specific somatic symptoms. This helps to make the interpretation of the findings reproducible (cf. Köneke 2005).
Table 1 provides a comprehensive summary of this classification model.
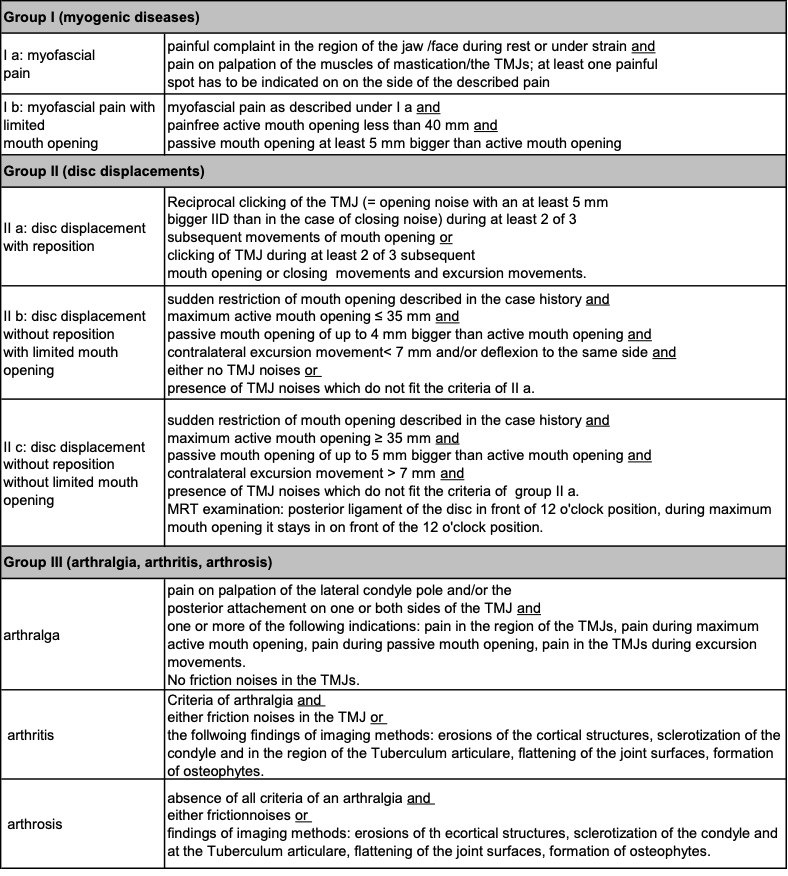
Table 1: Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD),
Dworkin and LeResche, 1992
Since the CRAFTA® therapy concept in part relates to this classification system, this model was used as a basis for the examination of the patients in this study.
The functional interrelations between the stomatognathic system and the rest of the body are multi-layered and extremely complex. Due to numerous clinical studies the interrelations between functional disturbances of the TMJ and problems in the locomotor system are in general sufficiently well known, but direct structural and neurophysiological connections are controversially discussed (cf. Bumann et al. 2000, Madsen 2005, Schupp 2005). In addition, there is no homogeneous, comprehensive and scientifically proven model which provides a guideline and explanation. This makes the CMD multi-facetted and difficult to understand, especially since there is no clear prime symptom (cf. Ahlers et al. 2007).
The connections that are relevant for this paper are briefly presented below. Regarding a comprehensive overview the reader is asked to refer to Schupp (2005) and Madsen (2005). Basically, the knowledge about the connections is either the result of empirical observations and pilot studies or can be regarded as theoretical models only. In addition, often only a partial aspect is covered. Thus the result is a fragmented picture of sometimes complementary knowledge, where the TMJ plays a central role.
From the orthopaedic perspective there are the following descriptions of anatomical and neurological connections:
- Rocabado (1983) describes a biomechanical connection between the head, neck and hyoid regions. In this context the infra- and suprahyoidal muscles are of great importance. These two groups of muscles have a great influence on the curve of the cervical spine. If they are in balance the craniovertebral articulations remain in their normal position and the TMJ has an ideal contact with the cranial base.
- According to von Treuenfels (1984) a prognathy of the maxilla or an extremely open bite is in up to 30% of the cases the cause of an atlas-inferior position. This corresponds to an extension position of the Os occipitale, with an approximation of the Arcus vertebralis atlantis posterior and the Os occipitale. The resulting stretch of the ligaments between the Arcus vertebralis atlantis anterior and the Dens axis can ensue a narrowing of space for the cerebrospinal fluid in the subarachnoid space and can negatively affect the Aa. Vertebralis, the cranial and spinal meninges, the Medulla oblongata and the adjacent nuclei of the N. hypoglossus, the Ganglion cervicale superius as well as the N. vagus.
- According to Clark et al. (1993) dysfunctions of the shoulder girdle can have an effect on the TMJ via the connection of the M. omohyoideus to the hyoid bone and via the suprahyoidal muscles or via the M. sternocleidomastoideus and its connection with the Os temporale.
- According to today’s knowledge of the functional connections of the TMJ, which links the lower jaw with the head, Kopp et al. (2000) consider the TMJ as the superior cranial joint. For them the craniomandibular system has a direct functional link with the craniocervical system via the muscle-fascia apparatus.
- Sieber et al. (2003) showed in an examination that there is a closer correlation between stress and muscle tension than there is between stress and any other CMD-sign. A significant correlation could be observed between emotional strains and the muscle index but not between emotional strains and the index for articular symptoms.
- Neuhuber (2004) described that the occipito-cervical junction and the tone of the cervical muscles are closely linked with the position and the function of the TMJ. The head is carried in such a way that the teeth optimally fit together. In addition, the muscles of mastication are also used to stabilize the cervical spine.
A glance at the available osteopathic literature reveals the following connections, which represent the empirical knowledge of the osteopaths and/or have only the character of a model.
- According to Magoun (1975) the Ossa temporalia play a key role in the occlusion of the mouth. On the one hand they are part of the cranium and on the other hand they are directly influenced by the visceral system. Magoun calls the Ossa temporalia: “Troublemaker in the Head (…) Structural deviations of these bones may be responsible for migraine headaches, vertigo, strabismus, and malocclusion of the teeth as well as bruxism and nystagmus.” (Magoun 1974, 825).
- Frymann (1983, 595) sees the following connections: “Temporomandibular joint dysfunction may produce local symptoms of pain, or noise in the joint, or objective findings of pronounced malocclusion, impaired excursion in the opening of the mouth, or deviant motions of the jaw in speech. In a far greater number of patients its symptoms may be more remote from the mouth or side of the head, and objective signs may be detected in any part of the body, from tenderness over the sagittal suture to an imbalance in leg lengths. Restoration of anatomic-physiologic function to the TMJ may favourably influence these distant pathologies. Conversely, correcting a short leg or addressing a factor that may be a common denominator of the TMJ imbalance and the presenting complaint may restore the TMJ to physiologic function.”
- Milne (1999, 42) explains that “The condition of the mandibular muscles has an effect from the tip of the greater wing of the sphenoid down to the tips of the toes.” He also thinks that this influence can happen the other way round. For instance, all muscles that have an influence on the scapula also have an effect on the stomatognathic system.
- According to Liem (2000) there is an interrelation between the masticatory system and the rest of the body via myofascial chains, which is represented in Figure 6.
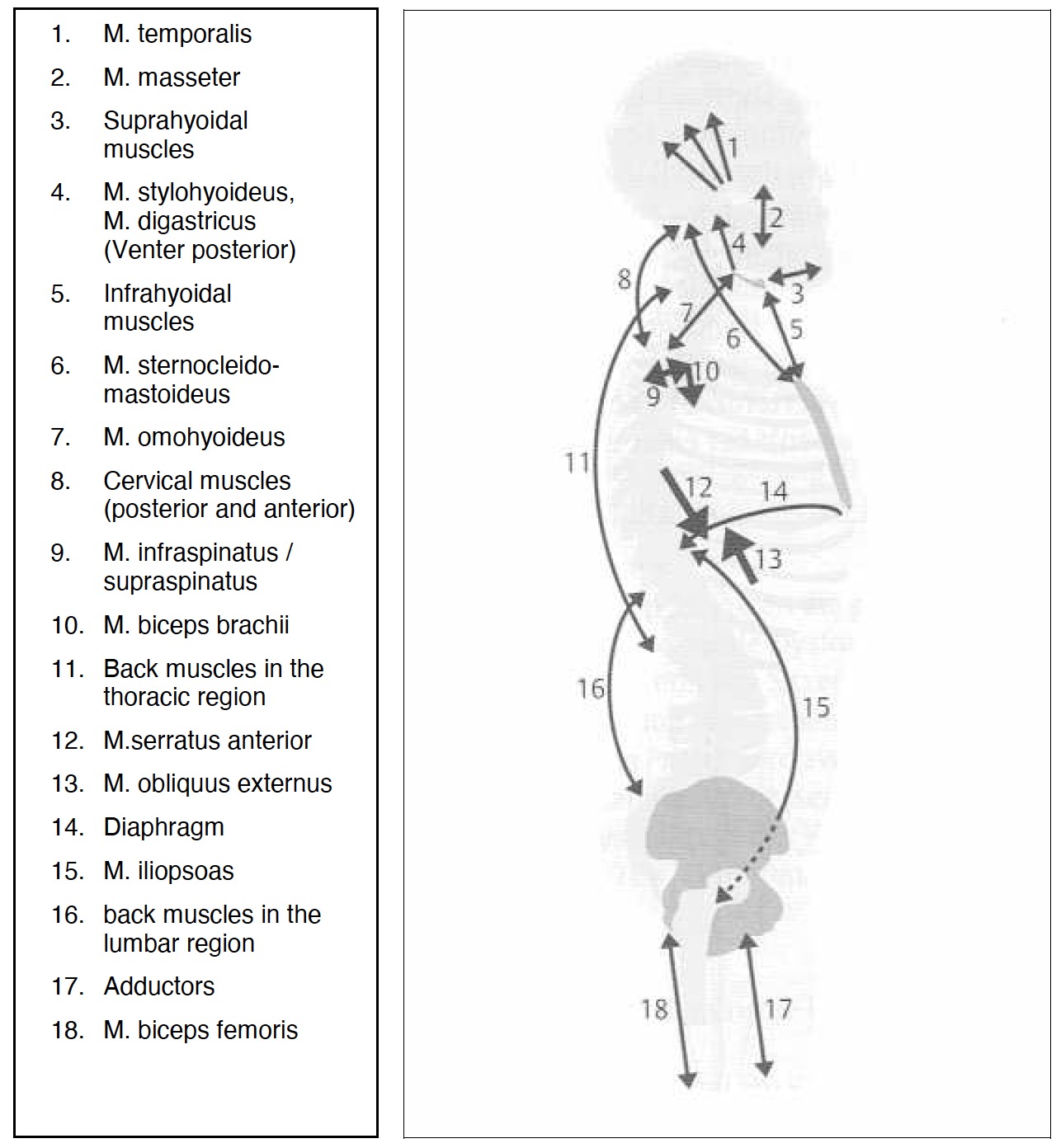 |
Figure 6: Interrelations of TMJ and body via myofascial chains,
Liem, 2000, page 297
For Gohl-Fronmayer (2005) the visceral system, which begins with the correct swallowing, and its overall function have an influence on the function of the stomatognathic system just like respiration or the speech pattern.
Treatment of craniomandibular dysfunctions
It has already been pointed out in the introduction and the previous chapters that for the treatment of patients with CMD, the symptoms and interrelations are very complex and can have multi-causal origins. Therefore, there are numerous possibilities (cf. also Figure 1) by different medical specialities to treat CDM. Below (cf. Table 2) only osteopathy and manual therapy (whose effectiveness will be compared in this paper) are described and compared in more detail.
| Osteopathy | Manual Therapy (according the CRAFTA® concept) | |
| Definition: | Osteopathy is an independent holistic form of medicine which grasps the human being with all the multi-layered structural, functional and biochemical interrelations. | Manual Therapy according to the CRAFTA® concept is a therapy concept which deals specifically with CMD complaints and their treatment around the regions of the head, neck, throat and face. |
| Approach: | Black Box Approach | Black Box Approach |
| Treatment- region: | The whole body as a unit, which is devided into the:Parietal systemVisceral systemCraniosacral system | TMJCranial bonesCervical spineCranial nervous systemMuscular structures in the region of the head and neckPelvis (secondary) |
| Treatmenttechniques: | Basically all osteopathic treatment techniques can be applied.They can be divided into:Parietal techniquesVisceral techniquesCraniosacral techniques | The typical treatment techniques of manual therapy can be applied:TractionTranslationMobilisationManipulationin addition the CRAFTA®-specific techniques can be applied:CompressionMuscular soft tissue techniques like stretching, cross-fibre friction, trigger point treatmentNeurodynamic mobilisation |
Table 2: Comparison of osteopathy with manual therapy (CRAFTA ® concept)
for the treatment of patients with CMD
For more information regarding other therapy possibilities for the treatment of patients with craniomandibular dysfunctions the following authors can be recommended to start with:
- Pharmacological therapy: von Lindern 2000, Kares et al. 2001,Umstadt 2002, Kehr 2005, Gündel et al 2006
- Occlusal correction / orthodontics: Bumann et al. 2000, Hippel 2006
- Acupuncture: Grandjean 2003, Gleditsch 2004
- Surgical interventions: Sanders 1988, Sader 2005
- Psychotherapy: Kluckhuhn 2006, Ahlers et al. 2007
The present work is a clinical pilot study. Its design, implementation and statistical analysis are described below. Basically, a clinical study evaluates the influence of a medical treatment approach for a disease on human beings in a controlled experimental environment (cf. Johannsen 2008). In this case the effectiveness of an osteopathic treatment is evaluated in comparison with a manual treatment (according to the CRAFTA® concept) for patients suffering from craniomandibular dysfunctions.
To guarantee an optimal result a randomized controlled trial (RCT) was chosen, which is regarded as the best study design in medical research for the evaluation of the effectiveness of certain methods. An RCT represents the classical implementation of experimental logics into clinical research, which means that its evidence has to be valued more than that of other study types. Thus the RCT takes the first rank among primary studies, the so-called “gold standard” (Scherfer 2005).
In the present study the potential participants were first of all checked with regard to defined inclusion and exclusion criteria. On the one hand this should guarantee that the symptoms are relevant, treatable and measurable, on the other hand it should make sure that equivalent preconditions are created for the comparison of the two therapy forms (osteopathy and manual therapy according to the CRAFTA® concept).
Eligible patients were then randomly divided into two groups. This prevented a conscious or unconscious manipulation in the preparation phase and allowed an equal distribution of known and unknown influencing factors among the two groups. One group served as the study group and its members were treated with osteopathy. The other group represented the comparison group and its members were treated with manual therapy according to the CRAFTA® concept.
Every patient received the same number of treatments within a set period of time and following a previously defined procedure. During the course of the treatments the necessary data for the evaluation and comparison was collected. The results are presented in Chapter 4 and compared and causally interpreted in Chapter 5. In this chapter possible differences between the two groups are attributed to the applied treatment method, which allows evaluating the effectiveness of osteopathy and manual therapy (according to the CRAFTA® concept) for the treatment of patients with craniomandibular dysfunctions.
Selection and allocation of the patients
To recruit the patients for this study selected dentists, ENT specialists, orthopaedists and speech therapists in the area of Düsseldorf were contacted. They received a brief explanation of the background and objective of this study with the request to mention towards appropriate patients the possibility of a free participation in this study. During a first phone call/conversation the potential participants received information about the purpose, objective and background of the study. In addition, it was checked whether they fit the inclusion and exclusion criteria. Eligible patients were then randomly divided into the two groups and a first appointment was arranged.
The patients who finally were included in this study were all older than 18 years, German-speaking and suffering from the relevant CMD symptoms for more than 6 months. During the study period they did not receive any other treatment by a physical therapist, osteopath or dentist and they fulfilled at least three of the following five inclusion criteria:
- Pain in the region of the muscles of mastication
- Bruxism (grinding) or bracing (compressing)
- Deviation when opening the mouth
- Restricted ability to open the mouth
- Clicking sounds when opening the mouth
These inclusion criteria were chosen because:
- they are the typical cardinal symptoms of CMD (cf. Ahlers et al. 2007)
- they can be easily measured (cf. Chapter 3.3)
- they are in general treatable by means of physical therapy (cf. Fink 2000)
- they have already been applied in numerous studies and examinations on the topic of CMD, e.g. Nikolakis el al. 2001, Hülse et al. 2003, Knust 2006, Van Assche 2006 and von Pickartz 2007.
Potential patients for this study were excluded if they showed the following symptoms:
- Pronounced dysgnathia
- Facial pain caused by systemic, neurological or psychiatric diseases
- Acute or chronic TMJ trauma
- Sinusitis
The exclusion criteria were supposed to guarantee that no therapy-resistant patients could distort the results, that all patients could be treated with both therapy methods and that no contraindications were present.
Randomized allocation of the patient into the two groups
After the verification of the inclusion and exclusion criteria the eligible patients were randomly divided into the following two groups:
- OST group = study group osteopathy; treatment delivered by Ms Anett Hörster and
- MT group = comparison group manual therapy according to the CRAFTA® concept; treatment delivered by a certified CRAFTA® therapist
To guarantee the necessary randomization a One-Euro coin was flipped at the occasion of the first encounter (cf. Kool et al. 2001). Patients who got the result “Number” were attributed to the OST group and those who got the result “Eagle” were attributed to the MT group. The patients were thoroughly informed about the study and the free participation but they did not receive any information about the division into the two groups and the differences between the two therapies.
Examination and treatment of the patients
Every patient was treated three times within a period of two weeks following a Black Box approach and the procedure defined below. Between the first and second treatment was at least one day but maximal 5 days, while between the second and third treatment were at least 4 and maximal 8 days. These basic definitions should guarantee that all patients (thus both groups) were treated under the same frame conditions. The patients were invited to come at least ten minutes earlier to the appointments to relax before the start of the actual treatment.
1st Appointment, approx. 90 minutes
- Welcome
- Explanation of the study and declaration of consent, approx. 5 minutes
- Case history, approx. 10 minutes
- Completion of the SES (pain perception) and SF36 questionnaire, approx. 15 minutes
- VAS assessment, approx. 2.5 minutes
- Biofeedback EMG measurement, approx. 15 minutes
- IID measurement and control of deviation, approx. 2.5 minutes
- Examination, approx. 10 Minuten
- Treatment depending on the examination findings, approx. 25 minutes
- Period of rest, approx. 5 minutes
- Good bye
- 2nd Appointment, approx. 60 minutes
- Welcome
- Control examination, approx. 10 minutes
- Treatment according to examination findings, approx. 45 minutes
- Period of rest, approx. 5 minutes
- Good bye
3rd Appointment, approx. 90 minutes
- Welcome
- Control examination, approx. 10 minutes
- Treatment according to examination findings, approx. 35 minutes
- Period of rest, approx. 5 minutes
- Biofeedback EMG measurement, approx. 10 minutes
- VAS assessment, approx. 2.5 minutes
- IID measurement, approx. 2.5 minutes
- Completion of SES (pain perception) and SF36 questionnaire, approx. 15 minutes
- Conversation concerning advice, approx. 5 minutes
- Good bye
- Final documentation, approx. 5 minutes
Measurement parameters and methods
Pain is the symptom that prompts the patients most often to search for treatment and visit their doctor (cf. Köneke 2005, Wicker Klinik 2008). Therefore is pain the most important measurement parameter in this clinical study. In addition to the measurement and analysis (of the change) of the acute pain intensity (VAS assessment) and of the pain perception / quality (SES questionnaire) also the health-related quality of life (SF36 questionnaire) of the patients is considered. This should allow for a better holistic consideration of the patient’s condition and thus leave more scope for the assessment in particular regarding the effectiveness of the osteopathic treatment.
Besides pain two additional measurement parameters were selected which help to evaluate typical CMD complaints and which, in contrast to the subjective pain assessment by the patients, can be objectively and reproducibly measured by the therapist. One of these parameters is the maximum opening of the mouth (IID measurement) which can be experienced, if restricted, as a quite uncomfortable condition in everyday life. The other additional parameter is the increased muscle tension of the M. masseter during rest (Biofeedback EMG measurement) which is supposed to be influenced by bruxism, bracing and/or pathological body statics, but like restricted mouth opening must not be painful.
Pain, VAS assessment and SES (pain perception) questionnaire
In contrast to other sensory perceptions like seeing or hearing, pain cannot be measured objectively and easily because it strongly depends on emotional factors and is a very subjective experience. Therefore various documentation systems can be used to facilitate and standardize the communication between the patient and the physician or therapist. Besides body diagrams to localize the pain so-called Visual Analogue Scales (VAS) are used to assess the pain intensity just like various questionnaires to evaluate the different dimensions and influencing factors of pain (cf. Köneke 2005).
In this study all three documentation systems were applied. While the body diagram was only used in the process of examination and diagnosis, the actual pain intensity was assessed with the VAS and the pain quality over a longer period of time (several days) was evaluated by means of the pain perception scale (SES questionnaire according to Geissner 1996). The results of the latter two methods were analysed. Both methods play a central role in the diagnosis and as a progression parameter of CMD, in particular when they are combined (cf. Stibenz 2004).
VAS assessment
Basically, visual analogue scales (VAS) can be regarded as a variant of the modality comparison, where the subjective pain intensity is depicted as a line of a certain length. The line has defined ends, e.g. “no pain” and “worst possible pain”. Visual analogue scales have therefore the characteristic of a ratio scale, i.e. percentage changes in the pain intensity can also be interpreted. Moreover, they have proven to be a reliable and valid measuring method to quantify the pain intensity (cf. Rosenow et al. 2004).
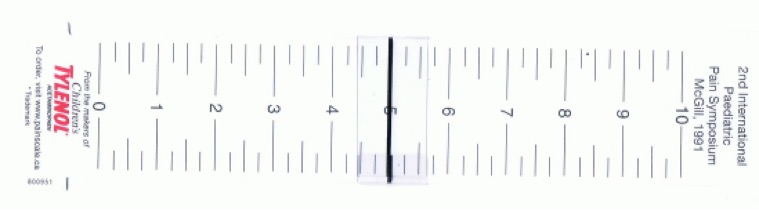
In this clinical study the subjective pain intensity was measured using the VAS by the company Painscale (cf. Figure 7). With the aid of a “pain slider” the patient indicated his/her perceived pain intensity on a ca. 10 cm long bar. The increase of the pain intensity from one end of the bar representing “no pain” to the other end of the bar representing “most pain” is also illustrated by an increasing width of the bar and the intensity of its red colour. The patient’s indicated pain intensity was read off the back of the VAS. The scale ranges from 0 = “no pain” to 10 = “most pain” and is divided into 0.25 intervals. The patients were always asked in a resting position about their pain perception.
The VAS assessment proved to be a quite easy, quick and straightforward method and did not require a lot of explanation to the patients. It could be carried out in about 2.5 minutes at the beginning of the first and at the end of the last treatment session, where the patients were asked to consider and assess only the relevant pain in the head, throat and neck region. The results were directly recorded on the individual patient’s examination sheet.
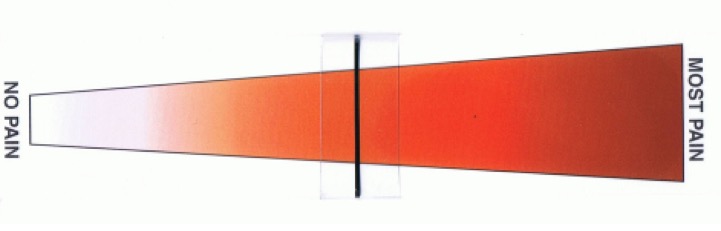
Figure 7: Visual Analogue Scale by the company Painscale
SES questionnaire (pain perception)
The pain perception scale (SES questionnaire) facilitates a multi-dimensional, differentiated evaluation of subjectively experienced chronic and acute pain. The scale can be used for various different forms of pain or diseases which entail pain. It enables not only a differentiated description of the perceived pain but also allows the evaluation of changes due to analgic therapy measures, which also include manual and physical therapeutic treatments and exercises. The pain perception scale (SES questionnaire) used is appropriate for German-speaking pain patients (male and female) aged between 16 and 80 (cf. Geissner 1996).
The SES consists of a questionnaire comprising 24 items. All the items are attributed to five traits (scales): two traits describe the affective aspects of the perceived pain (expressing a feeling, i.e. concerning the psychic component of the pain, the aspect of suffering) and three traits describe the sensory aspects of the perceived pain (the sensory quality, i.e. the physically perceived component of the pain).
The traits are described with different descriptors and are summarized in two global dimensions (SES Global-Affective or SES Global-Sensory). Any further aggregation to obtain an overall pain value does not make sense neither from a statistical nor from a content point of view (cf. Geissner 1996). The first 14 items represent the affective aspects (Part A) and the following 10 items represent the sensory aspects (part B) of the SES (cf. Table 3).
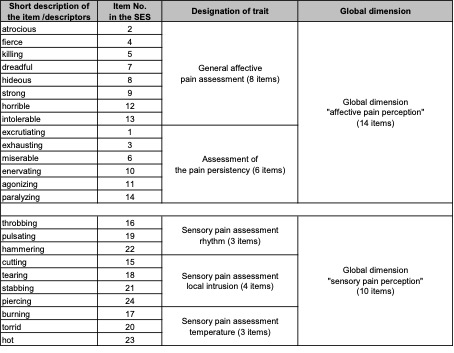
Table 3: Overview of items, traits and global dimensions of the SES, Geissner, 1996
For the description of the pain, i.e. for answering the questions of the SES, the following three different time frames can be selected: “in the last 3 months”, “in the last few days” and “in this moment”. To evaluate the effectiveness of specific interventions the time frame “in the last few days” is recommended (cf. Geissner 1996). Therefore the patients in this study were told to consider this period when answering the questions.
The answers to the 24 items depend on the degree of each individual’s agreement with the pre-defined statements, i.e. the degree of correspondence of the personal situation with the pre-defined statements for the chosen time frame. The patients have to evaluate for each item whether the statement fits to their perceived pain by choosing from four standard answers: “does totally apply” (= 4 points), “does apply to a large extent” (= 3 points), “does apply to a lesser extent” (= 2 points) or “does not apply” (= 1 point). All items are oriented in the same direction, i.e. the more intensive the pain the higher the points.
After completion of the questionnaire, the points are added to calculate the results for the five traits (scales) first. Then the global dimension “affective pain perception” (SES Global-Affective) is calculated by adding the defined 14 affective items (Item
1 to 14 = Part A of the SES). The same applies for the calculation of the global dimension “sensory pain perception” (SES Global-Sensory) (Item 15 to 24 = Part B of the SES). The range of the calculated results depends on the number of items and the individual answers of the patients. In the case of the global dimension “affective pain” it ranges from a minimum of 14 to a maximum of 56 points, while for the global dimension “sensory pain” it ranges between a minimum of 10 and a maximum of 40 points.
There is no set time limit for answering the SES questionnaire. In the present clinical study the patients needed about 5 to 10 minutes. Attention was paid that the patients completed all questions and that they filled in their name, the date and their therapist (to have a reference to the treatment group). The patients had to answer the questionnaire before the first and after the last treatment session and were asked to consider and evaluate only the relevant pain in the regions of the head, throat and neck.
Quality of life, SF36 questionnaire
The health-related quality of life can be equalized with subjective health indicators and refers to a multi-dimensional construct, which has to be parameterized by at least four components: the mental wellbeing, the physical condition, the social relations and the functional competency of the patients. In general, this construct is accepted for evaluating treatments (cf. Bullinger et al. 1998).
The SF36 is a questionnaire that was specifically developed to evaluate this health-related quality of life. It is appropriate for patients aged 14 years and older. Like for the SES questionnaire, it is also important for the SF36 that the patients themselves provide the information about their wellbeing and their ability to function.
The SF36 comprises a total of 36 items referring to 8 different health concepts and regarding changes in the stat of health (cf. Table 4). The topics include questions about physical function, role physical, bodily pain, general health, vitality, social function, role emotional, mental health and changes in the state of health
(cf. Bullinger et al. 1998).
Three different versions of the SF36 questionnaire are available: a self-assessment questionnaire, a third-party assessment questionnaire and an interview sheet. In addition, it is differentiated according to the time frame taken into account: the “standard version” with a time frame referring to the last 4 weeks and the “acute version“ with a time frame referring to the last week. The “acute version“ of the SF36 self-assessment questionnaire was chosen for the present study. The reason for this choice was that the assessment should be carried out without any third party influence (self-assessment) and a “before-after“ comparison for an overall treatment period of only two weeks (“acute version”) was intended.
| Summaries | Health concepts | Number of items | Description |
| Physical summary scale | Physical function | 10 | Degree to which the state of health impairs physical activities like self-sufficiency, walking, climbing stairs, bending, lifting and moderate or vigorous activities |
| Role physical | 4 | Degree to which the physical condition limits work or other daily activities, e.g. accomplish less than usual, limitations in the kind of activity or difficulties performing certain activities | |
| Bodily pain | 2 | Degree of pain and influence of pain on normal work inside or outside the home | |
| General health | 5 | Personal assessment of the general health including the current state of health, future expectations and resistance against diseases | |
| Mental summary scale | Vitality | 4 | To feel full of energy and drive vs. tired and exhausted |
| Social function | 2 | Degree to which the physical health or emotional problems influence normal social activities | |
| Role emotional | 3 | Degree to which emotional problems limit work or other daily activities; e.g. to have less time, to accomplish less, to work less carefully as usual | |
| Mental health | 5 | General mental health including depression, fear, emotional and behaviour-related control, general positive attitude | |
| Changes in the state of health | 1 | Evaluation of the current state of health in comparison to a certain period of time (4 weeks/ last week) |
Table 4: Overview and description of the summary scales and health concepts of the
SF36 questionnaire, Bullinger 1998, page 12
For each of the 36 items the patient’s task in the questionnaire is to choose the answer that comes closest to his/her personal experience for the specified period. In contrast to the SES questionnaire the categories of possible answers vary. There are questions that offer only binary answers, i.e. the questions can be answered e.g. with either “yes“ or “no“ and other questions that offer scales of up to six different answer possibilities.
The analysis of the SF36 questionnaire is carried out with a special computer program, which transforms the scales of the health concepts into values between
1 and 100, applies a weighting and adds up the values. In this way the results for the various health concepts can be calculated. They can also be summarized into an overall physical summary scale and mental summary scale. Only the changes in the state of health are not transformed and are always considered separately.
In general, there is no set time limit for the completion of the SF36 questionnaire. The patients in this study needed about 10 to 15 minutes. Attention was paid that the patients completed all questions and that they filled in their name, the date and their therapist (to have a reference to the treatment group). The patients had to answer the SF36 questionnaire before the first and after the last treatment session.
Mouth opening, IID measurement
A restricted (active) mouth opening is always present when a patient’s mobility of the lower jaw is objectively reduced, which is a typical symptom of CMD. It can be painful but this does not necessarily have to be the case. Even though the normal, healthy mouth opening and thus also a possible restriction can vary from person to person, the literature indicates a “scientific limit“. This ranges around 40 mm to 42 mm
(cf. Bumann et al. 2000, Stelzenmüller et al. 2004). In the present clinical study a “restricted mouth opening” is understood as a maximum active mouth opening that is smaller than 40 mm.
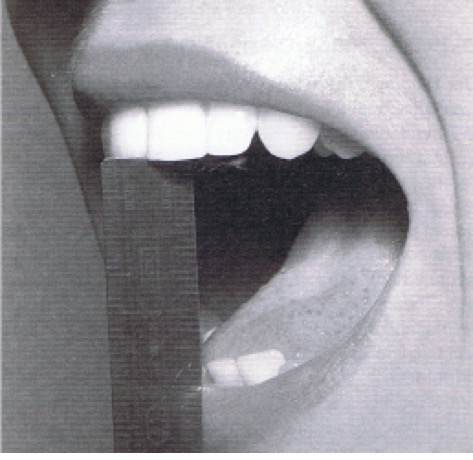
The mouth opening is usually measured as the distance between the incisors (inter-incisor distance, IID). The patient has to (actively) open his/her mouth as far as possible and the therapist positions a solid ruler between the edge of the upper incisors and the edge of the lower incisors. The maximum active mouth opening can now be determined on the ruler in millimetres by the therapist (cf. Figure 8). Such an IID measurement is objective and reproducible. Many studies have shown that the reliability of such a measurement ranges from moderate to good (cf. von Piekartz 2005).
In practice the IID measurement could be carried out quickly and easily. The patients’ mouth opening was measured before the first and after the last treatment and the values were recorded in millimetres on the examination sheets.
Figure 8: IID measurement with a ruler
von Piekartz, 2005, page 138
Muscle tension, Biofeedback EMG measurement
The tension in a muscle is also called muscle tone. It has a passive viscous-elastic component and an active component which is determined by the muscle contraction (cf. Mense 1998). The contractile component can be measured quite well for the skeletal muscles because an active contraction of a muscle produces among others an electric field on the skin (cf. Dittel 1992). In the following the term muscle tension is used to describe this active contractile component which is linked with the muscle’s contraction and which can be measured as an electric charge.
A healthy skeletal muscle in a totally relaxed state does not have any muscle tension at all, i.e. no fibres contract. If this state cannot be achieved despite all relaxation efforts, the muscle is in a pathologic electrogenic spasm (cf. Mense 1998). This state can be but does not necessarily have to be painful.
In this clinical study the muscle tension of the M. masseter (on the left and right side) were measured because patients with CMD often have an increased tension in this muscle (cf. Slavicek et al. 1995) and the muscle tension or changes of it have proven to be a meaningful diagnostic criterion in the case of CMD. The progression of the disease and the success of the treatment can be controlled and documented very well due to the objectivity and reproducibility of this measurement method (cf. Huelse et al. 2003).
A biofeedback device was used to measure the muscle tension. In general, biofeedback is understood as a therapeutic procedure where body functions, which we are not or hardly conscious of, are measured with the aid of apparatuses. The patient receives an optic or auditory feedback of these biological signals. This can help patients to influence these physiological processes in a targeted way to positively change them. (cf. Korn 2005).
Biofeedback devices can be used to measure e.g. skin conductance, pulse amplitude, pulse frequency, temperature, respiration, electrical activity of the brain and the muscle tension. In this clinical study the biofeedback device was only used to measure the muscle tension.
The measurement, analysis and documentation of the muscle tension is also called electromyography (EMG). It looks at changes in the electrical state on the surface of the muscle fibres, the so-called action potentials, which depend on de-polarization and re-polarization processes (cf. Konrad 2005). The fluctuations of these potentials can be measured with electrodes that are attached to the surface of the skin or with needle electrodes that are inserted into the specific muscle. While needle electrodes are mainly used to examine neurological problems, the surface electrodes are mainly applied to examine the activity progression and the interaction of several muscles or muscle groups.
The surface EMG is regarded as reliable if the muscles to be measured are not covered by others and are situated directly under the skin (cf. Ettlin et al. 1998)
– like it is the case with the M. masseter.
In this study the two-channel EMG module of the Biofeedback 2000 x-pert device by the company Schuhfried was used. The one-way adhesive electrodes Blue Sensor M by the company Ambu were used as surface electrodes (cf. Figure 9).

Figure 9: EMG module of the Biofeedback device 2000 x-pert by the company Schufried
and one-way adhesive electrode Blue Sensor M by the company Ambu
The muscle tensions of the M. masseter on the right and left were measured at the same time with two electrodes applied on each side (two-channel device). The difference between the two electrodes on the left and the difference between the two electrodes on the right side were measured (bipolar conduction). The reference electrode was always applied to an electrically uninvolved (neutral) spot at the neck. The biofeedback device amplified, demodulated and averaged the signals using a time constant of 250ms (cf. Schuhfried 2006).
The results of such an EMG measurement are thus two time-averaged and demodulated interference curves (one for the left and one for the right M. masseter), which each represents an overlay of all measured action potentials of the corresponding muscle and which is indicated in microvolt.
A healthy and relaxed muscle does not show any EMG activity due to the lack of the membrane de-polarization and the associated action potentials. In theory the measuring result would be displayed as a flat baseline. In reality, however, a
so-called baseline noise occurs. It is caused by different disturbing signals or artefacts. These are for example external disturbing charges, changes in the distance between the muscle and the electrode (due to e.g. movement) or electrical signals from adjacent muscles (physiological cross talk).
In the case of modern EMG amplifiers and when the skin is optimally prepared the baseline noise should not exceed 3 to 5 microvolt. This cannot always be achieved in reality but nevertheless 1 to 2 microvolt have to be considered as optimum
(cf. Konrad 2005).
The EMG measurements were carried out before the first and after the last treatment of each patient. In every case the M. masseter left (with the dark green plug) and right (with the light green plug) were measured in a resting state. During each measurement three ten-second intervals were recorded. They were announced by the therapist so that the patients could observe the rules of behaviour described below.
Before the EMG measurement the skin of the patients was cleaned and degreased to obtain the best possible conductibility. Thereafter the M. masseter was palpated, the coordinates for the electrodes were determined and marked on the examination sheet (or taken from the examination sheet for the following measurements) to guarantee a reproducible measurement arrangement.
The coordinates of the first electrode in the region of the M. masseter were determined on an imaginary line between the Incisura intertragica and the beginning of the Sulcus nasolabialis. The distance to the Incisura intertragica was measured and recorded on the examination sheet. The coordinates of the second electrode were determined on an imaginary line between Angulus mandibularis and the Angulus oris. This distance was also measured and recorded (cf. Figure 10).
It has to be pointed in this context out that it is of advantage for an EMG measurement when both electrodes are placed on the muscle belly in the direction of its fibres. This ensures the best possible signals (cf. Konrad 2005). For all patients the electrical uninvolved cervicothoracal junction was chosen as position for the neutral electrode.
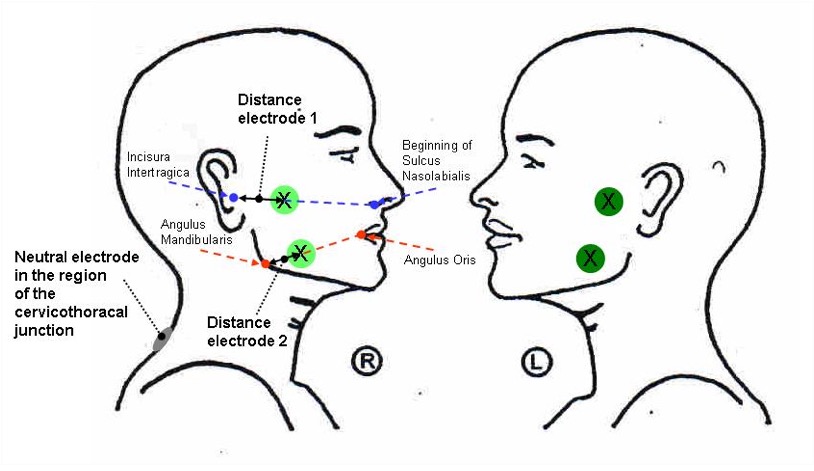
Figure 10: Determination, measurement and documentation of the coordinates
for the surface electrodes of the EMG measurement
After the five electrodes were applied at the determined spots and all cables were put into place, the patients were asked to respect the following rules of behaviour during the measurements in order to guarantee comparable and reproducible measurement conditions:
UPPM position (Upright Postural Position of the Mandible) (cf. von Pickartz 2005); which is characterized by:
- Sitting position
- Shoulders and head in neutral position
- Teeth slightly apart
- Lips closed but lips and chin relaxed
- Tongue relaxed, closely behind the upper incisors
Eyes closed and no view on the monitor
No swallowing or other movements
Even though the EMG module is a biofeedback device, the patients were not allowed to see the monitor at any time in order to avoid any possible training or habituation effects.
Figure 11 gives an example of such a biofeedback EMG measurement of the M. masseter left and right, where the results are depicted as a bar diagram, one above the other, for the relevant time period. The left side is shown in dark green above and the right side in light green below. The grey bars mark the start and end points for the defined three 10-second intervals. Between the intervals there was always a short break.
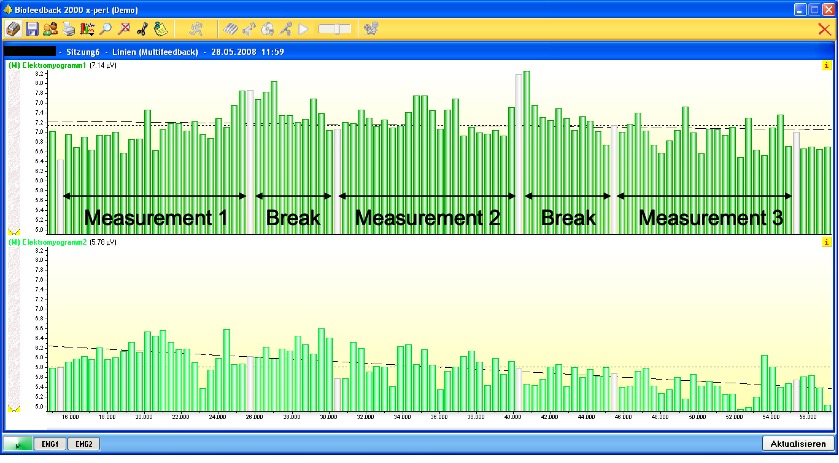
Figure 11: Example of an EMG measurement with the biofeedback device 2000 x-pert
by the company Schufried
Figure 12 gives an example for a comparison of the first measurement (left = before the first treatment – pre) and the second measurement (right = after the last treatment – post) for the left (dark green, above) and right (light green, below) side.
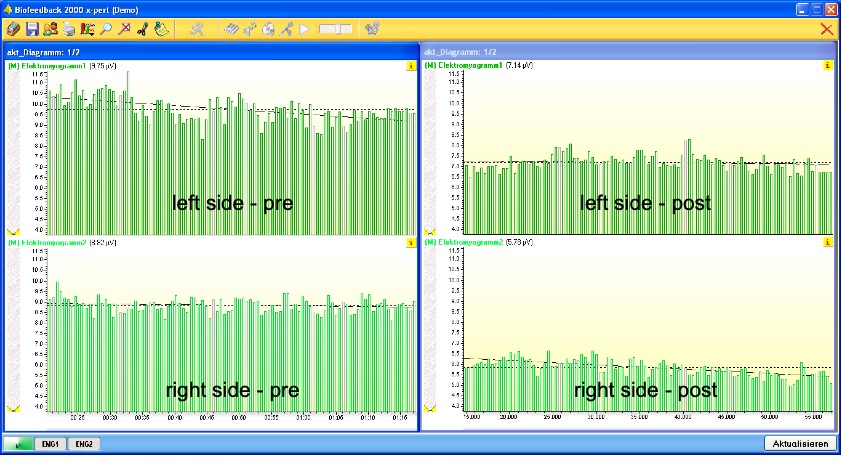
Figure 12: Example of a comparison of the first and second EMG measurement with the biofeedback device 2000 x-pert by the company Schufried
The computer programs Excel and SSPS (with the additional SF36 module) for Windows were used for the collection, analysis and graphical presentation of the obtained patient data. The IID and VAS values were gathered from the examination sheets and manually entered into Excel. Also the data from the SES and SF36 questionnaires were entered manually into Excel. It was possible to directly export the EMG values from the biofeedback software into Excel.
The collected data was then checked with the SPSS software to see whether certain distribution patterns could be observed, e.g. a Gaussian distribution. This was almost always the case so that the parametric T-test was used for the statistical analysis. Only for the traits rhythm and temperature of the SES questionnaire and for the health concepts role physical and social function of the SF36 questionnaire no distribution pattern could be found. Therefore non-parametric tests were applied for those cases; first the Wilcoxon test and afterwards the Mann-Whitney-U-test for the comparison of the OST group with the MT group. In addition, the reliability of the SES and SF36 questionnaires was verified. The Cronbach’s alpha was above the threshold of 0.7 for both the SES (Parts A and B) and the SF36 (physical and mental summary scale). Therefore the results of the two questionnaires could be considered as reliable (cf. Bullinger et al. 1998 und Geissner 1996).
Comparisons, trends etc. are generally regarded as “statistically significant” if the results cannot be attributed to mere coincidence. Usually the variable p is used to indicate the level of significance. If the level is small enough, the result can be taken as significant. For this clinical study a significance level of p=0.05 was chosen. One usually speaks about a highly significant result if p<0.01. For the analysis of the various measurement values (IID, VAS, SF36, SES, EMG) always the same procedure was observed. First of all, all patients were evaluated as a collectivity; then the OST and MT groups were analyzed separately to recognize changes (post vs. pre). Finally, these changes within the different groups were compared. The results are presented in tables and diagrams in Chapter 4 together with general patient analysis. In the boxplots the outliers and extreme values are marked as crosses. genug, spricht man von einem signifikanten Ergebnis. Für diese Arbeit wurde ein Signifikanzlevel von p=0,05 ausgewählt. Von hochsignifikant spricht man üblicherweise wenn p<0,01 ist. Bei der Auswertung der verschiedenen Messwerte und Daten (SKD, VAS, SF36, SES, EMG) wurde immer die gleiche Reihenfolge verwendet. Zunächst wurden alle Patienten als Gesamtheit und darauf die Gruppen OST und MT separat auf Veränderungen untersucht (post zu pre). Zum Schluss wurden dann die Unterschiede der beiden Gruppen miteinander verglichen. Die Ergebnisse sind als Tabellen und Graphiken zusammen mit einer allgemeinen Patientenauswertungen im Kapitel 4 dargestellt. Bei den Boxplots sind die Ausreißer- und Extremwerte als Kreuzchen dargestellt.
The treatments for this clinical study were carried out between March and July 2008. A total of 21 patients participated in the study, but one female patient had to be excluded and was not considered in the statistical analysis due to a botox injection into the M. masseter. The remaining 20 patients all received three treatments within a period of two weeks according to the procedure defined in Chapter 3.2. The patients were randomly divided into the two groups, the OST and the MT group, which turned out to be of the same size by coincidence (cf. Figure 13).
Figure 13: Distribution of the patients
The average age of the patients was 40.8 years, with a range from 19 to 65 years
(cf. Figure 14).
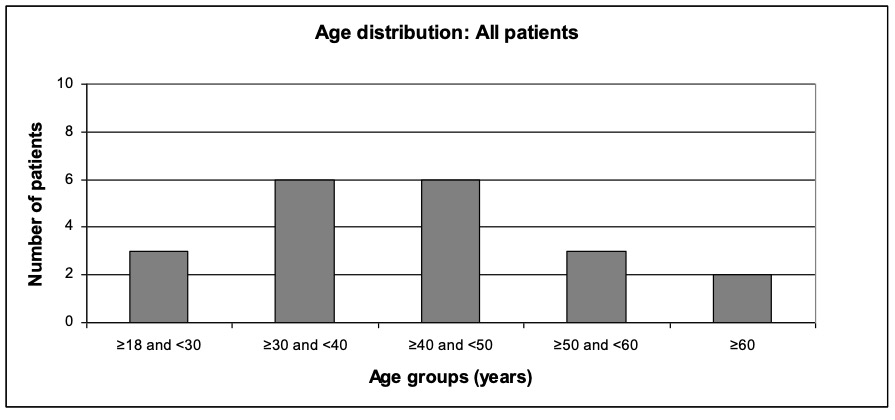
Figure 14: Age distribution: All patients
The average age of the OST group was 39.1 years, with a range from 21 to 57 years (cf. Figure 15).
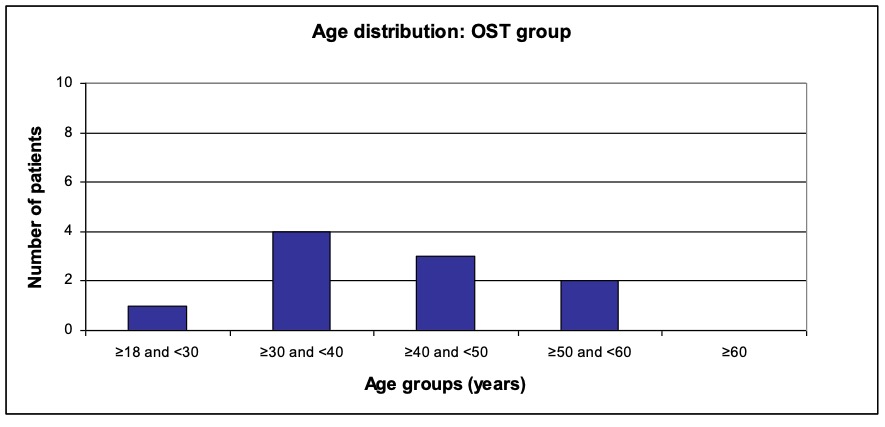
Figure 15: Age distribution: OST group
The average age of the MT group was 42.5 years, with a range from 19 to 65 years (cf. Figure 16).
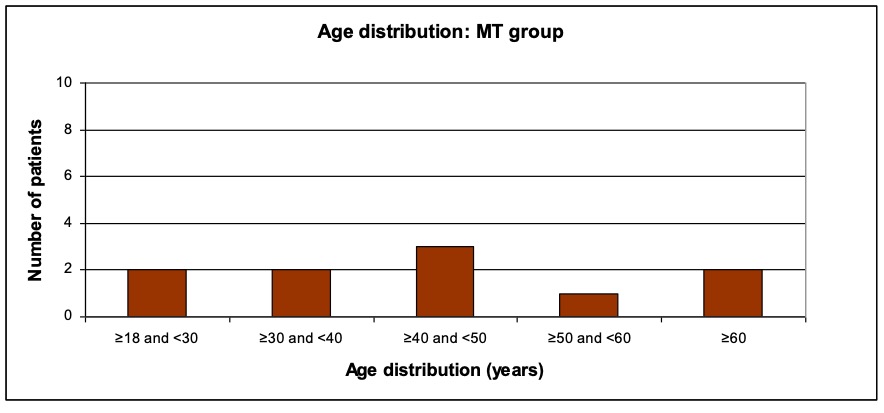
Figure 16: Age distribution: MT group
18 of the patients were female and 2 male and each treatment group consisted of 9 female and 1 male test persons. The gender distribution of all patients is illustrated in Figure 17.
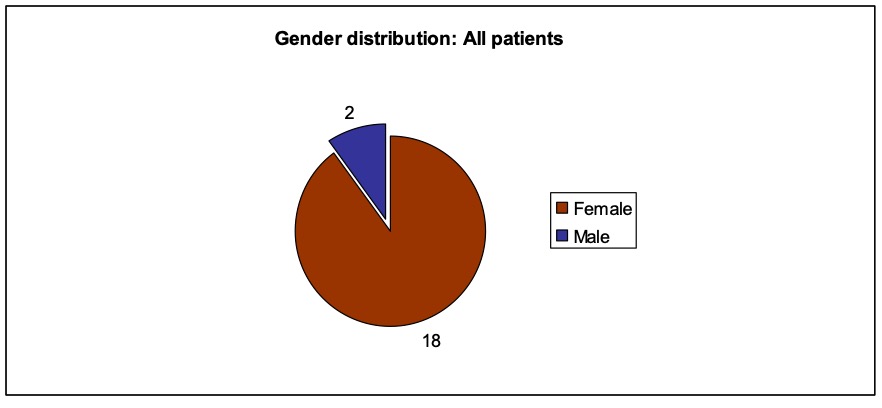
Figure 17: Gender distribution: All patients
All patients fulfilled at least 3 of the 5 defined inclusion criteria. With the exception of the inclusion criterion restriction (restricted mouth opening) all inclusion criteria occurred more or less similarly often (cf. Figure 18).
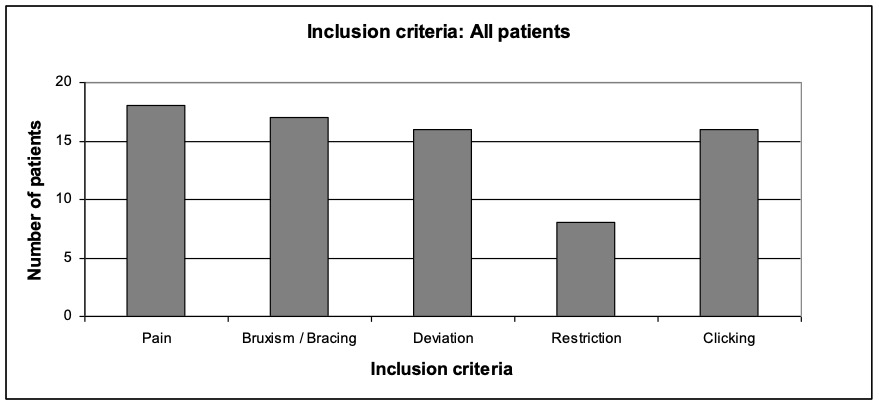
Figure 18: Inclusion criteria: All patients
In the OST group pain and bruxism/bracing were the most frequent inclusion criteria. All 10 patients of the OST group named this criterion. Slightly less (but by the same amount) deviation and clicking were indicated. Only every second patient indicated restriction as an inclusion criterion (cf. Figure 19).
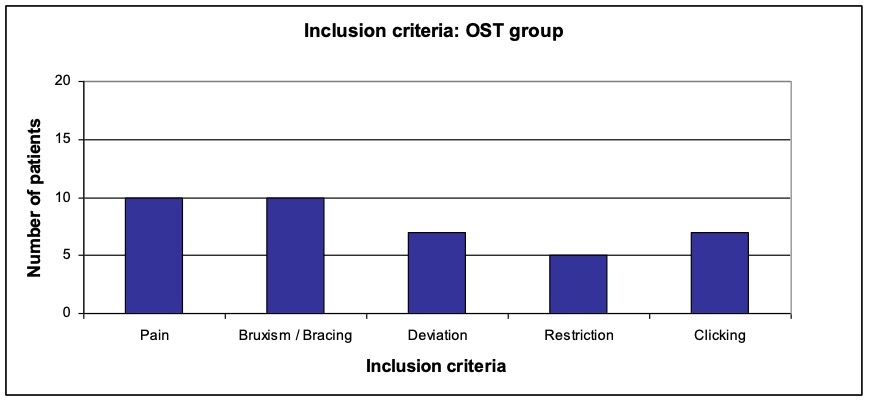
Figure 19: Inclusion criteria: OST group
In the MT group all inclusion criteria except restriction occurred in approximately the same number (cf. Figure 20).
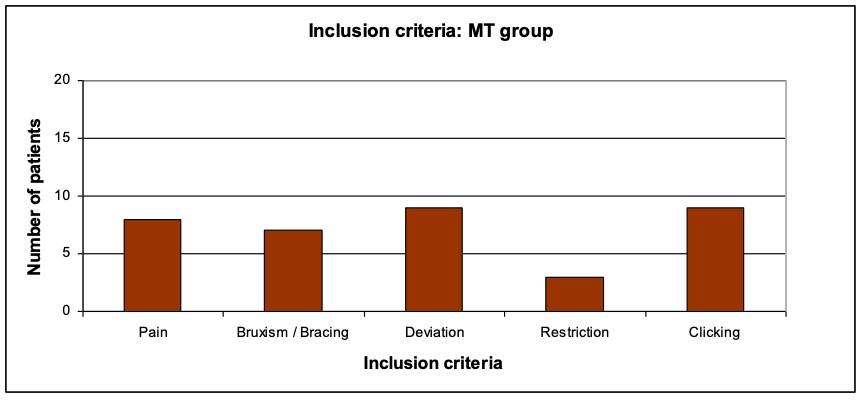
Figure 20: Inclusion criteria: MT group
At the beginning of the course of treatments the mean value (pre) of all patients in the VAS assessment was 4.07. Due to the treatments a mean improvement (reduction) of -1.53 and thus a mean value (post) of 2.54 could be achieved. With p=0.000 this was a highly significant improvement for all patients (cf. Table 5).
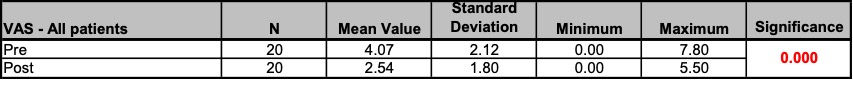
Table 5: VAS – All patients: Results; Unit of measurement: Points
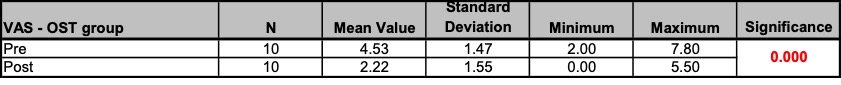
Before the treatments the mean value (pre) in the VAS assessment of the OST group was 4.53. Through the osteopathic treatment a mean improvement of -2.31 and thus a new mean value (post) of 2.22 could be achieved. With p=0.000 this was a highly significant improvement for the OST group (cf. Table 6).
Table 6: VAS – OST group: Results; Unit of measurement: Points
Figure 21 illustrates the pre and post VAS values of all patients of the OST group.
All patients displayed a clear improvement due to the osteopathic treatment.
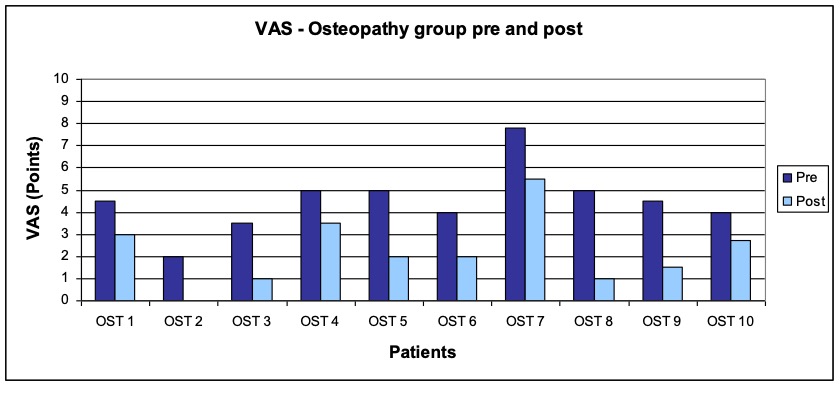
Figure 21: VAS – OST group pre and post
Before the treatments the mean value (pre) in the VAS assessment of the MT group was 3.60. Through the manual therapy (according to the CRAFTA® concept) a mean improvement of -0.75 and thus a new mean value (post) of 2.85 could be achieved. However, with p=0.057 this improvement was marginally not significant for the MT group (cf. Table 7).
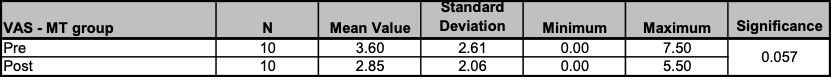
Table 7: VAS – MT group: Results; Unit of measurement: Points
Figure 22 illustrates the pre and post VAS values of all patients of the MT group. Two patients (MT 1 and MT 9) did not had any complaints right from the start (and non at the end), while one patient (MT 5) experienced a slight deterioration (increase) after the treatments.
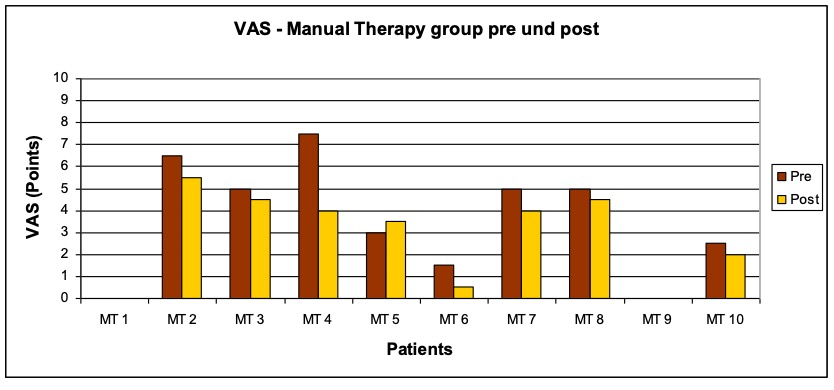
Figure 22: VAS – MT group pre and post
Figure 23 shows a graphic comparison of the pre and post VAS values for all patients, for the OST group and the MT group in a boxplot diagram. What is noticeable in particular was the clear improvement of the OST group in comparison with the MT group.
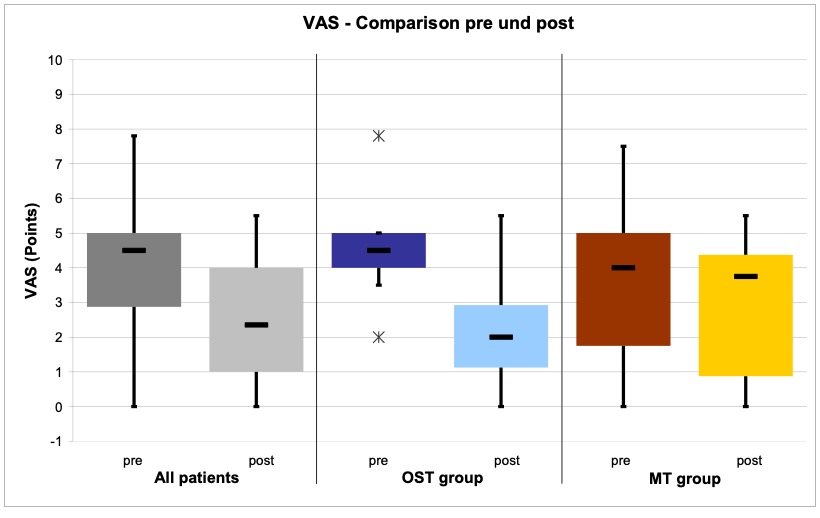
Figure 23: VAS – Comparison pre and post
In the OST group a mean improvement of -2.31 could be observed, while the mean improvement in the MT group was only -0.75. This means that in comparison with the manual therapy (according to the CRAFTA® concept) osteopathy was more effective. With p=0.002 this difference was highly significant. (cf. Table 8).
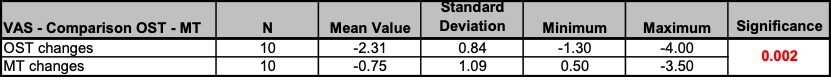
Table 8: VAS – Comparison OST – MT; Unit of measurement: Points
Figure 24 provides a graphic comparison of this result, illustrating the changes of the VAS values for all patients, for the OST group and the MT group in a boxplot diagram. A reduction (negative value) corresponds to an improvement.
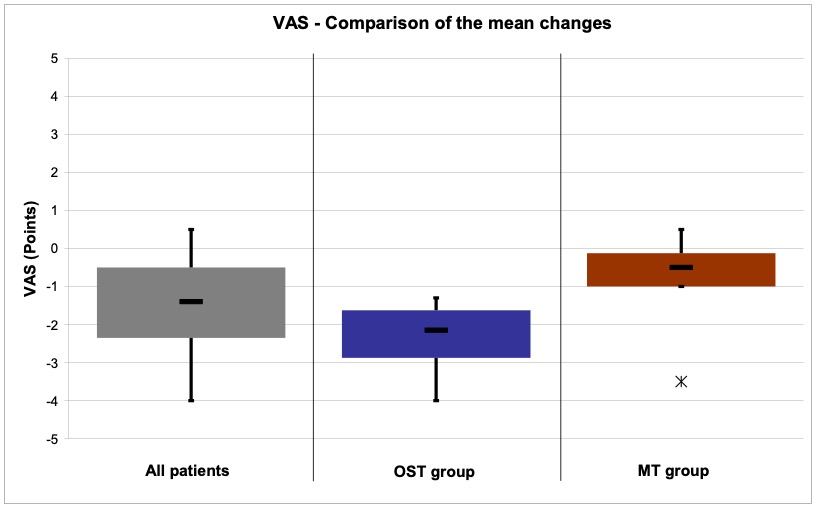
Figure 24: VAS – Comparison OST – MT
At the beginning of the course of treatments the mean value (pre) of all patients for the SES questionnaire was 22.55 for the global dimension affective, while it was 14.85 for the global dimension sensory. Due to the treatments a mean improvement (reduction) of -4.60 and thus a mean value (post) of 17.95 could be achieved for the global dimension affective, while a mean improvement of -2.30 and thus a mean value (post) of 12.55 could be observed for the global dimension sensory. With p=0.001 each, this represents a highly significant improvement for all patients for both global dimensions. Also the traits that are summed-up in the global dimensions showed significant improvements (with the exception of the temperature). Further details can be gathered from Table 9.
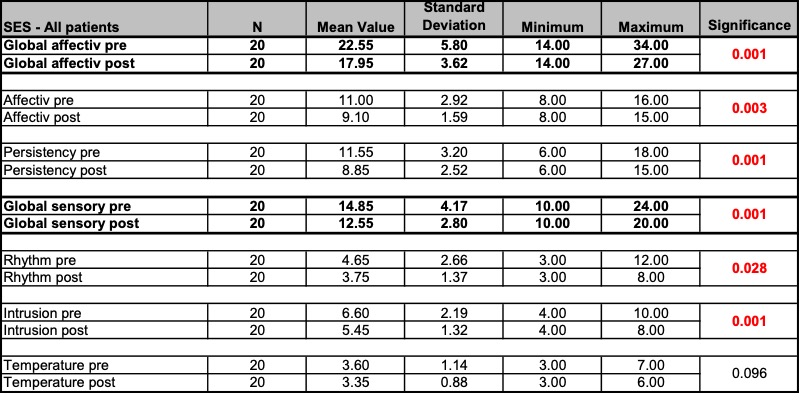
Table 9: SES – All patients: Results; Unit of measurement: Points
Before the treatments the mean value (pre) of the OST group in the SES questionnaire was 24.50 for the global dimension affective, while it was 16.60 for the global dimension sensory. The osteopathic treatment could achieve a mean improvement of -6.40 and thus a mean value (post) of 18.10 for the global dimension affective, while a mean improvement of -3.50 and thus a mean value (post) of 13.10 could be observed for the global dimension sensory. With p=0.006 and p=0.004 both global dimensions of the SES questionnaire displayed a highly significant improvement for the OST group. Also for the traits Affective and Persistency of the global dimension affective as well as for the trait Intrusion of the global dimension sensory a significant improvement could be observed in the OST group. Further details can be gathered from Table 10.
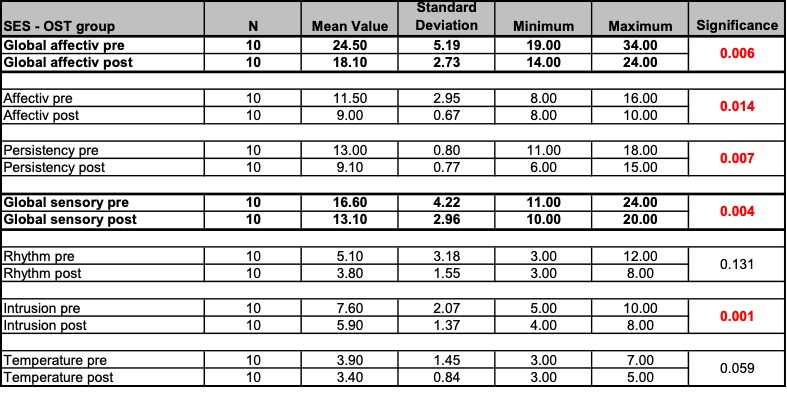
Table 10: SES – OST group: Results; Unit of measurement: Points
Figure 25 illustrates the pre and post values of the global dimension affective and sensory for all patients of the OST group. A clear improvement could be observed in almost all cases (with the exception of patient OST 6).
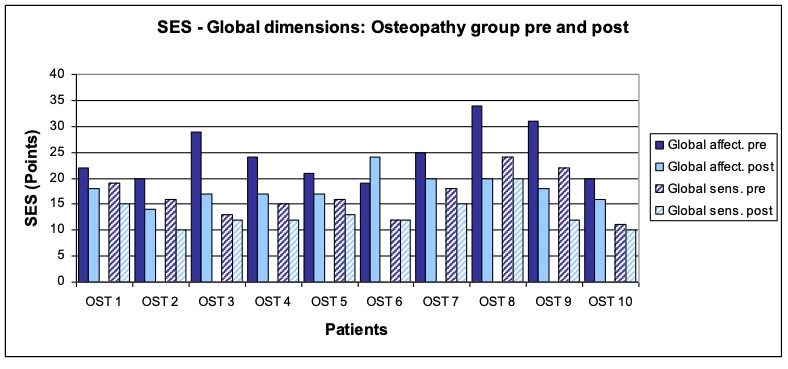
Figure 25: SES – Global dimensions: OST group pre and post
Figure 26 illustrates the pre and post mean values of the OST group for the global dimension affective with its traits Affective and Persistency as well as for the global dimension sensory with its traits Rhythm, Intrusion and Temperature. In almost all cases improvements could be observed, which all were significant (with the exception of Rhythm and Temperature).
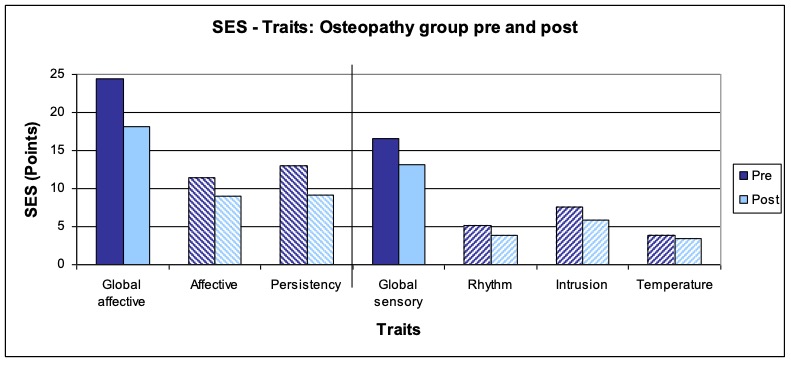
Figure 26: SES – Traits: OST group pre and post
Before the treatments the mean value (pre) of the MT group in the SES questionnaire was 20.60 for the global dimension affective and 13.10 for the global dimension sensory. With the manual therapy (according to the CRAFTA ® concept) a mean improvement of -2.80 and thus a mean value (post) of 17.80 could be achieved for the global dimension affective, while a mean improvement of -1.10 and thus a mean value (post) of 12.00 could be observed for the global dimension sensory. With p=0.032 this was a significant improvement for the MT group for the global dimension sensory, while with p=0.055 the improvement for the global dimension affective was marginally not significant. Regarding the various traits only Persistency showed a significant improvement in the MT group. Further details can be gathered from
Table 11.
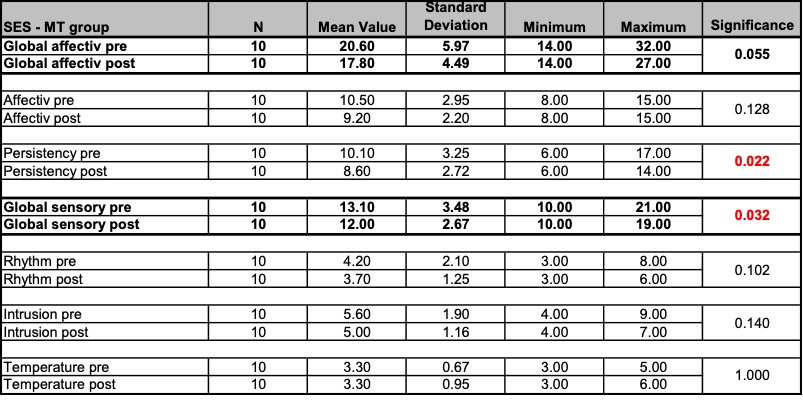
Table 11: SES – MT group: Results; Unit of measurement: Points
Figure 27 illustrates the pre and post values of the global dimensions affective and sensory for all patients of the MT group. About 50% of the patients experienced an improvement. In the case of some patients (MT 1, MT 7, MT 9) the values partly remained the same, while in the case of two patients (MT 5, MT 6) a deterioration (increase) in some values was be observed.
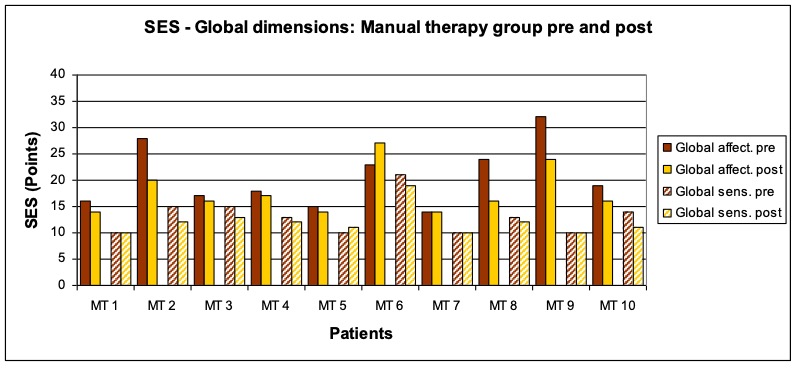
Figure 27: SES – Global dimensions: MT group pre and post
Figure 28 illustrates the pre and post mean values of the MT group for the global dimension affective and its traits Affective and Persistency as well as for the global dimension sensory with its traits Rhythm, Intrusion and Temperature. With the exception of the trait Temperature which remained unchanged improvements could be observed in all cases. However, they were only significant in the case of the global dimension sensory and the trait Intrusion.
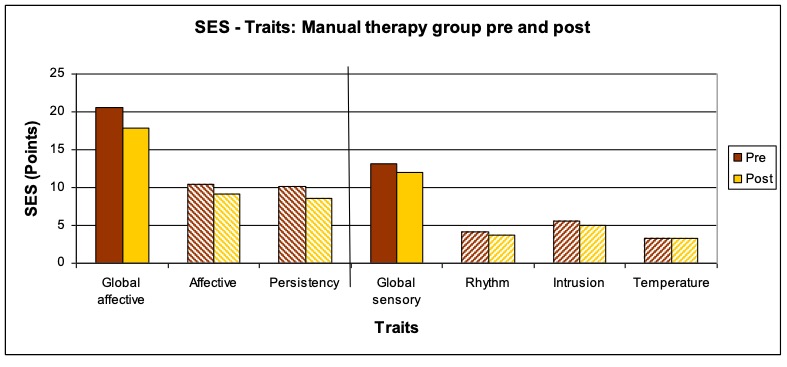
Figure 28: SES – Traits MT group pre and post
Figure 29 provides a graphic comparison of the pre and post SES values of the global dimensions affective and sensory for all patients, for the OST group and for the MT group in a boxplot diagram.
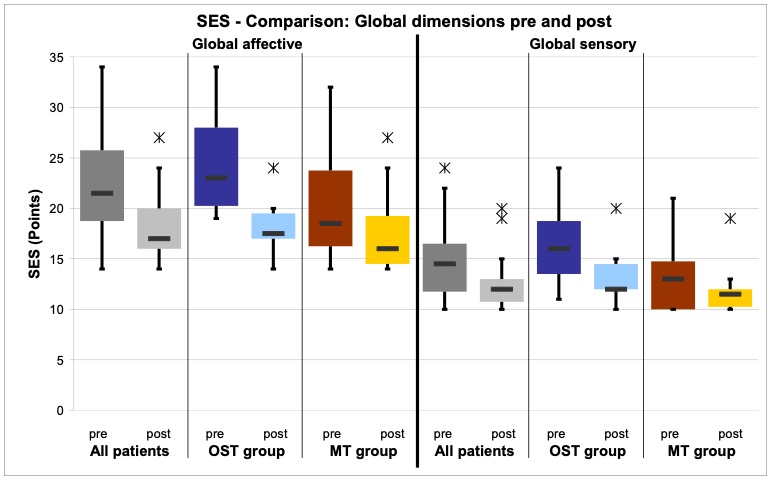
Figure 29: SES – Comparison global dimensions pre and post
Regarding the global dimension affective a mean improvement of -6.40 could be observed in the OST group, while the global dimension sensory improved only by an average of -3.50. In the MT group the global dimension affective improved on average by -2.80, while a mean improvement of -1.10 could be achieved for the global dimension sensory.
In comparison with the manual therapy (according to the CRAFTA® concept) osteopathy was significantly more effective (p=0.028) regarding the global dimension sensory and it was marginally significant (p=0.049) regarding the trait Intrusion. Concerning the global dimension affective and all other traits no significant differences could be observed comparing the effectiveness of the two treatment methods. Further details can be gathered from Table 12.
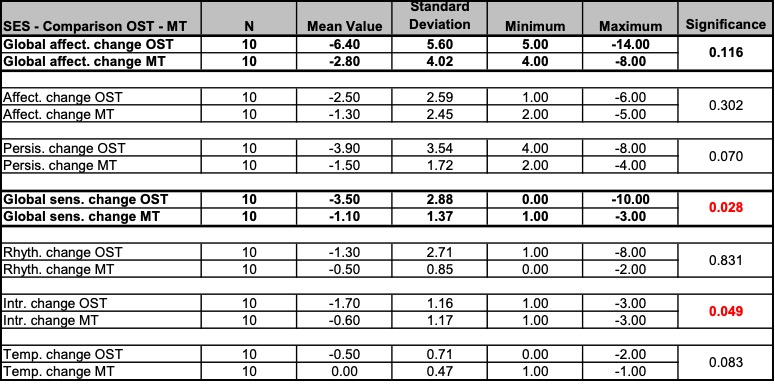
Table 12: SES – Comparison OST – MT; Unit of measurement: Points
Figure 30 provides a graphic comparison of the results, which illustrates the mean changes of the global dimensions affective and sensory of the SES questionnaire for all patients, for the OST group and for the MT group in a boxplot diagram.
A reduction (negative value) corresponds to an improvement.

Figure 30: SES – Comparison OST – MT
Quality of life, SF36 questionnaire
At the beginning of the course of treatments the mean value (pre) of all patients for the SF36 questionnaire was 46.04 for the physical summary scale and 46.43 for the mental summary scale. After the treatments a mean improvement (increase) of 3.61 and thus a mean value (post) of 49.65 could be observed for the physical summary scale. The mental summary scale improved on average by 3.88, which resulted in a mean value (post) of 50.31. With p=0.010 for the mental summary scale and p=0.054 for the physical summary scale, the improvement for all patients was significant for the first and marginally not significant for the latter. Among the 8 health concepts, which add up to the summary scales, more than half showed a significant improvement. For all the patients a highly significant improvement (reduction) of the change in health could be observed (p=0.004). Further details can be gathered from Table 13.
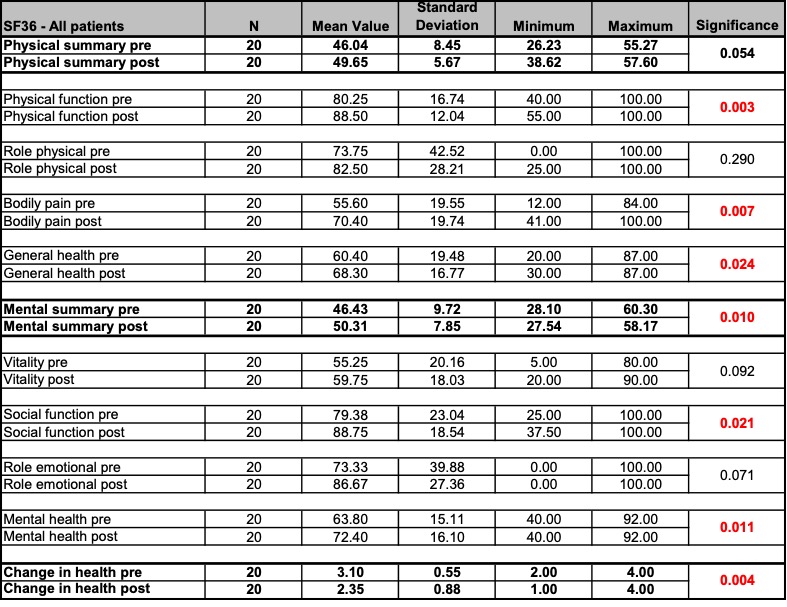
Table 13: SF36 – All patients: Results; Unit of measurement: (transformed) Points
Before the treatments the mean value (pre) of the OST group in the SF36 questionnaire was 43.67 for the physical summary scale and 41.59 for the mental summary scale. Through the treatments a mean improvement (increase) of 5.09 and thus a mean value (post) of 48.76 could be achieved for the physical summary scale, while the mental summary scale could be improved by an average of 8.96 to result in a mean value (post) of 50.55. With p=0.009 for the mental summary scale this represented a highly significant improvement for the OST group. Also the majority of the 8 health concepts, which add up to the summary scales, showed a significant improvement for the OST group (with the exception of role physical and role emotional). Regarding all patients of the OST group a highly significant improvement (reduction) could be observed for the changes in health (p=0.000). Further details can be gathered from Table 14.
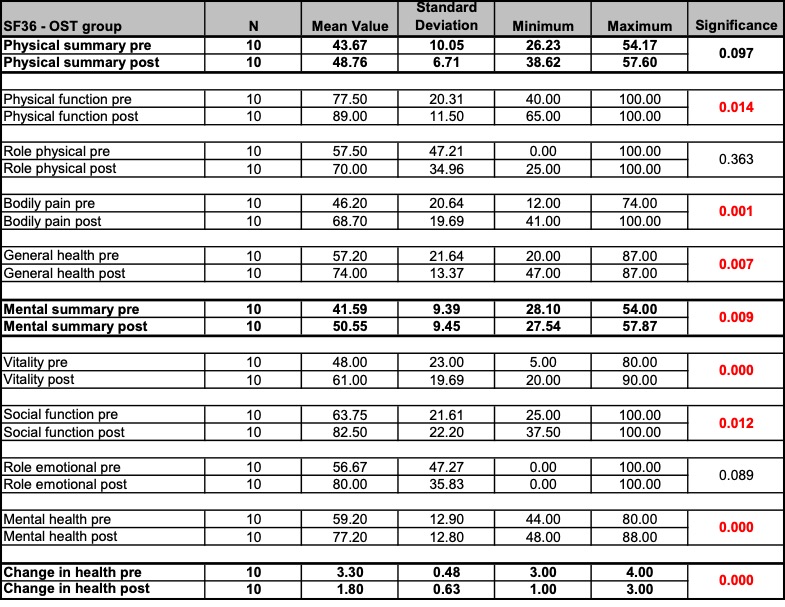
Table 14: SF36 – OST group: Results; Unit of measurement: (transformed) Points
Figure 31 illustrates the pre and post values of the physical summary scale and the mental summary scale for all patients of the OST group. An improvement (increase) could be observed in almost all cases (with the exception of patient OST1 andOST3).
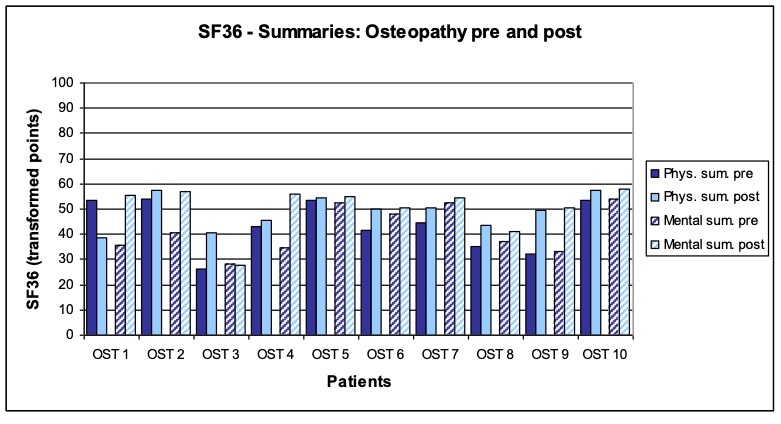
Figure 31: SF36 – Summaries: OST group pre and post
Figure 32 shows the pre and post mean values of the physical summary scale and mental summary scale for the OST group as well as the 8 health concepts, which add up to the summary scales. In all cases improvements could be observed. With the exception of the physical summary scale and the health concepts role physical and role emotional all improvements were significant.
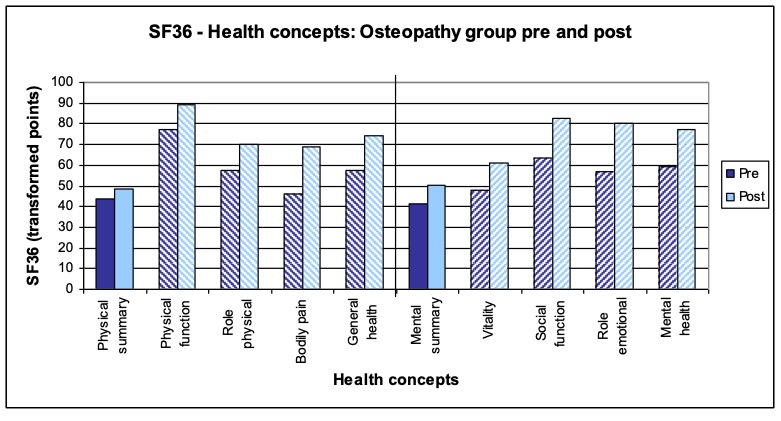
Figure 32: SF36 – Health concepts: OST group pre and post
Before the treatments the mean value (pre) of the MT group in the SF36 questionnaire was 48.42 for the physical summary scale and 51.27 for the mental summary scale. Due to the treatments a mean improvement (increase) of 2.13 and thus a mean value (post) of 50.55 could be achieved for the physical summary scale. The mental summary scale, however, clearly deteriorated (reduction) by a mean value of -1.2 which resulted in a mean value (post) of 50.07. Neither the improvement of the physical summary scale (p=0.365) nor the deterioration of the mental summary scale (p=0.388) were significant in the MT group. The 8 health concepts, which add up to the summary scales, showed a very inconsistent picture regarding improvements or deteriorations and none of the changes was significant. The patients of the MT group did not experience a change in their health due to the treatment. Further details can be gathered from Table 15.
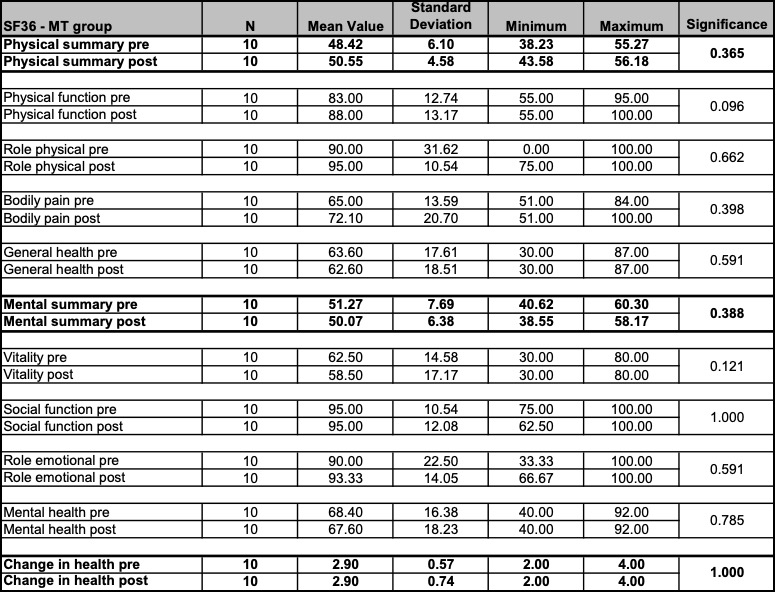
Table 15: SF36 – MT group: Results; Unit of measurement: (transformed) Points
Figure 33 illustrates the pre and post values of the physical summary scale and the mental summary scale for all patients of the MT group. A very inconsistent picture of improvements (increase) and deteriorations (reduction) could be observed.
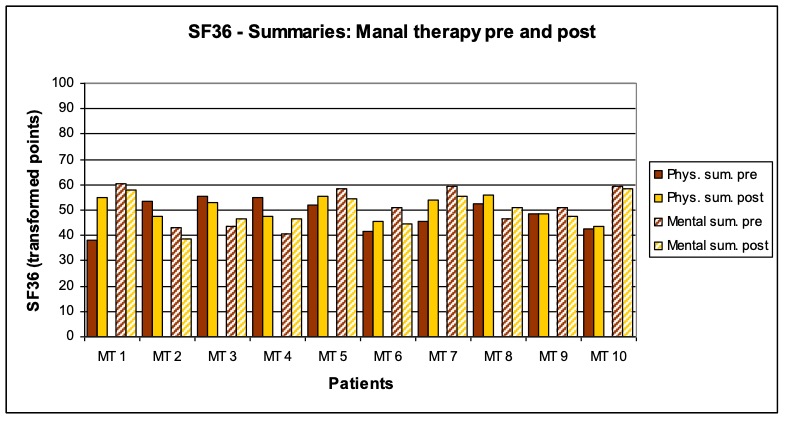
Figure 33: SF36 – Summaries: MT group pre and post
Figure 34 shows the pre and post mean values of the physical summary scale and the mental summary scale in the MT group as well as the 8 health concepts, which add up to the summary scales. Overall, a very inconsistent picture of improvements and deteriorations could be observed. None of the changes were significant.
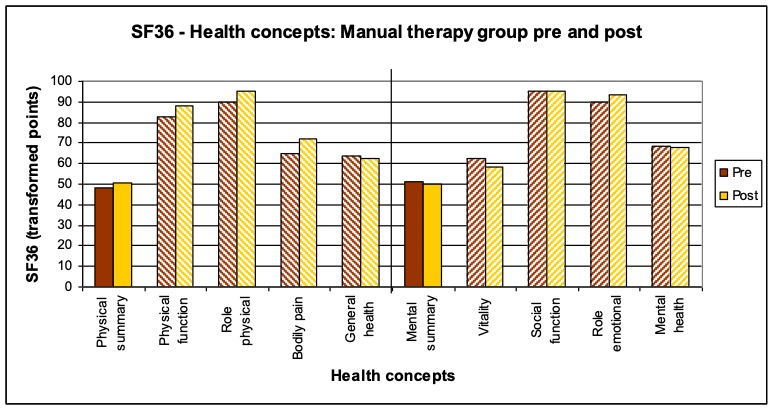
Figure 34: SF36 – Health concepts: MT group pre and post
Figure 35 provides a graphic comparison of the pre and post mean values of the physical summary scale and the mental summary scale for all patients, for the OST group and the MT group in a boxplot diagram.
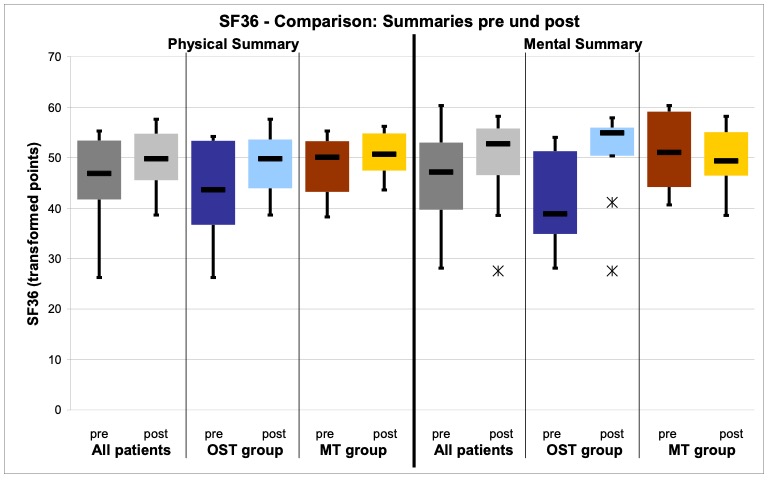
Figure 35: SF36 – Comparison: Summaries pre and post
For the OST group a mean improvement of 5.09 could be observed for the physical summary scale, while the mental summary scale improved by an average of 8.97. However, only the latter improvement was significant. For the MT group the physical summary scale only improved by an average of 2.13. Regarding the mental summary scale actually a mean deterioration of -1.20 could be observed, which, however, was not significant.
Compared with the manual therapy (according to the CRAFTA® concept) osteopathy was significantly more effective regarding the mental summary scale (p=0.03),
while it was marginally not significantly more effective regarding the physical summary scale (p=0.05). For half of the health concepts osteopathy was significantly more effective and in case of the changes in health with p=0.000 a highly significant better effectiveness could be observed. Further details can be gathered from
Table 16.
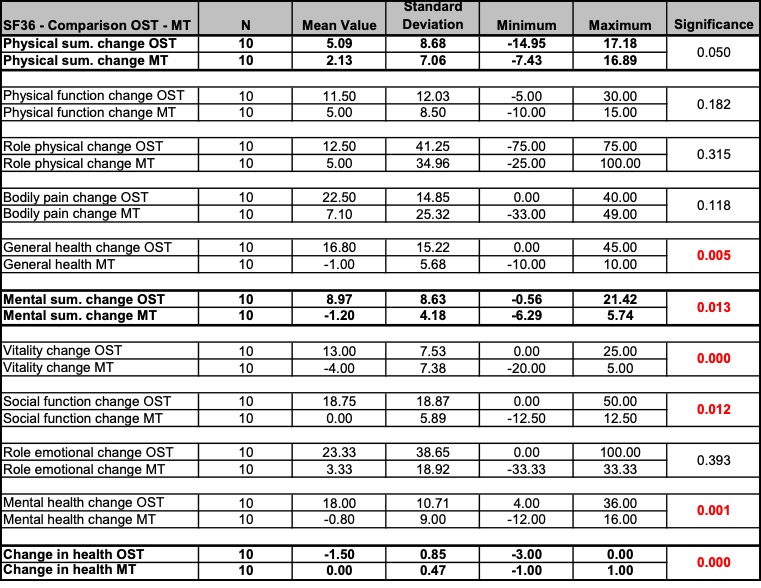
Table 16: SF36 – Comparison: OST – MT; Unit of measurement: (transformed) Points
Figure 36 provides a graphic comparison of the result, illustrating the average changes of the physical summary scale and the mental summary scale of the SF36 questionnaire for all patients, for the OST group and for the MT group in a boxplot diagram. An increase (positive value) corresponds to an improvement.
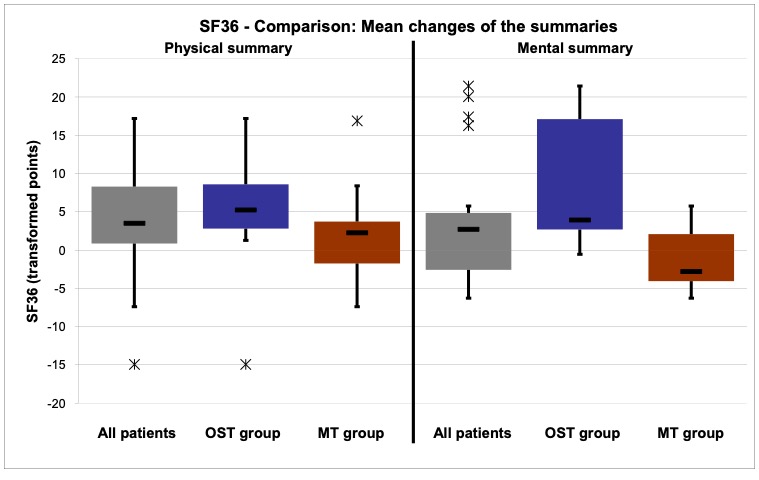
Figure 36: SF36 – Comparison OST – MT
Mouth opening, IID measurement
At the beginning of the course of treatments the mean value (pre) of all patients for the IID measurement was 40.80. After the treatments a mean improvement (increase) of 5.20 and thus a mean value (post) of 46.00 could be observed. With p=0.000 this was a highly significant improvement for all patients (cf. Table 17).
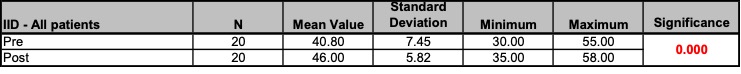
Table 17: IID – All patients: Results; Unit of measurement: Millimetres
Before the treatments the mean value (pre) of the OST group for the IID measurement was 37.70. Through osteopathy a mean improvement of 6.4 and thus a mean value (post) of 44.10 could be achieved. With p=0.000 this was a highly significant improvement for the OST group (cf. Table 18).
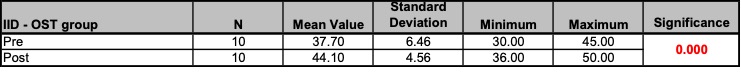
Table 18: IID – OST group: Results; Unit of measurement: Millimetres
Figure 37 illustrates the pre and post IID values for all patients of the OST group. Almost all patients showed a clear improvement after the treatment.
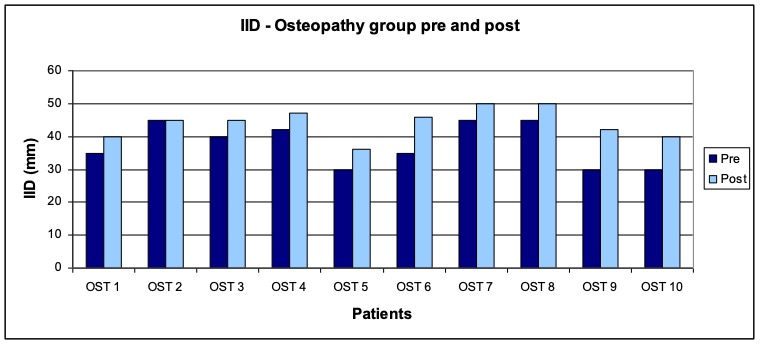
Figure 37: IID – OST group pre and post
Before the treatments the mean value (pre) of the MT group for the IID measurement was 43.90. Through the manual therapy (according to the CRAFTA® concept) a mean improvement of 4.00 and thus a mean value (post) of 47.90 could be achieved. With p=0.000 this was a highly significant improvement for the MT group
(cf. Table 19).
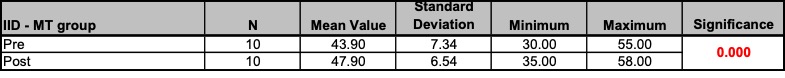
Table 19: IID – MT group: Results; Unit of measurement: Millimetres
Figure 38 illustrates the pre and post IID values for all patients of the MT group. Almost all patients showed a clear improvement after the treatment.
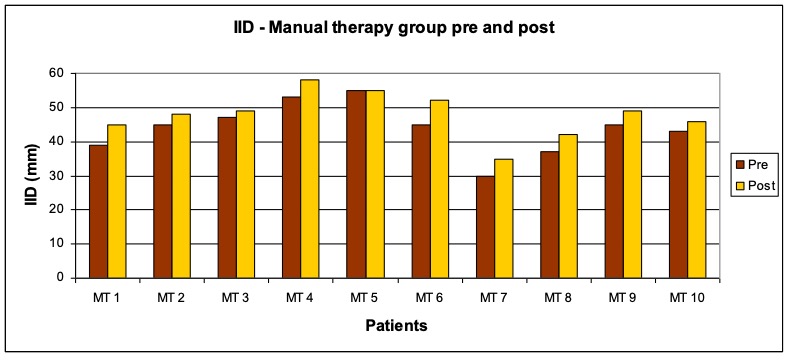
Figure 38: IID – MT group pre and post
Figure 39 provides a graphic comparison of the pre and post IID mean values for all patients, for the OST group and for the MT group in a boxplot diagram, which makes it easy to recognize the highly significant changes in both groups.
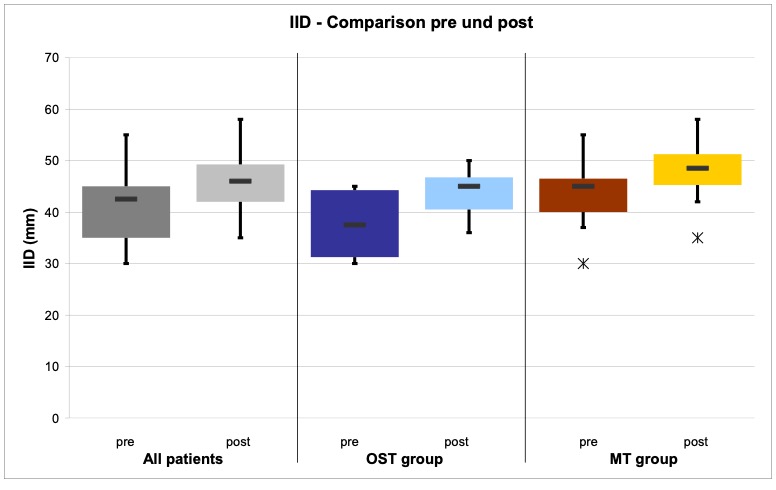
Figure 39: IID – comparison pre and post
For the OST group a mean improvement of 6.40 could be observed, while the MT group achieved a mean improvement of 4.0. Both improvements were highly significant Due to these successful results no real difference with regard to the effectiveness could be found between osteopathy and manual therapy (according to the CRAFTA® concept). Further details can be gathered from Table 20.
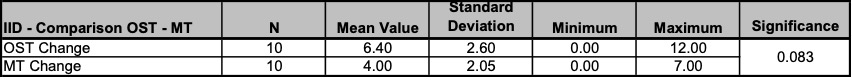
Table 20: IID – Comparison OST – MT; Unit of measurement: Millimetres
Figure 40 provides a graphic comparison of this result, illustrating the changes of the IID values for all patients, for the OST group and the MT group in a boxplot diagram. An increase (positive value) represents an improvement.
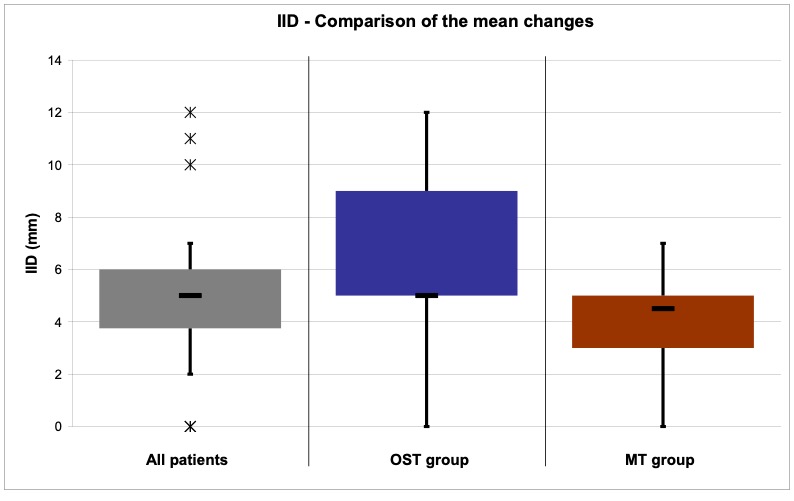
Figure 40: IID – Comparison OST – MT
Muscle tension, Biofeedback EMG measurement
At the beginning of the course of treatments the mean value (pre) of all patients for the EMG measurements was 4.78 on the left and 5.09 on the right side. Through the treatments a mean improvement (reduction) of -0.15 (left) and -0.84 (right) resulting in a mean value (post) of 4.63 (left) and 4.25 (right) could be achieved. This was with p=0.002 a highly significant improvement on the right side for all the patients
(cf. Table 21).
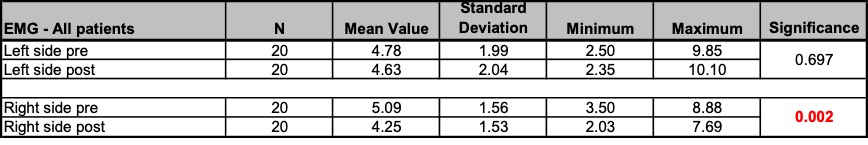
Table 21: EMG – All patients: Results; Unit of measurement: Microvolt
Before the treatments the mean value (pre) of the OST group for the EMG measurements was 4.98 (left) and 5.18 (right). Through the treatments a mean improvement (reduction) of -1.08 (left) and -1.10 (right) and thus a mean value (post) of 3.90 (left) and 4.08 (right) could be achieved. This result was a significant improvement for all the patients of the OST group on the left side with p=0.011 as well as on the right side with p=0.032 (cf. Table 22).
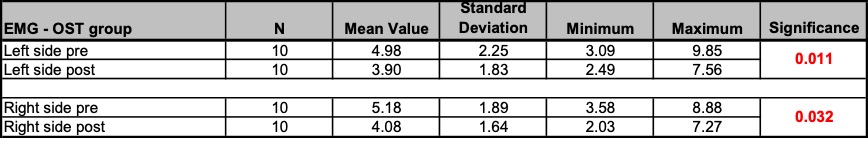
Table 22: EMG – OST group: Results; Unit of measurement: Microvolt
Figure 41 illustrates the pre and post EMG values on the left side for all patients in the OST group, while Figure 42 represents the same for the right side. Almost all patients showed an improvement (reduction) on both sides after the treatment (with the exception of OST 1, OST 2 and OST 3).
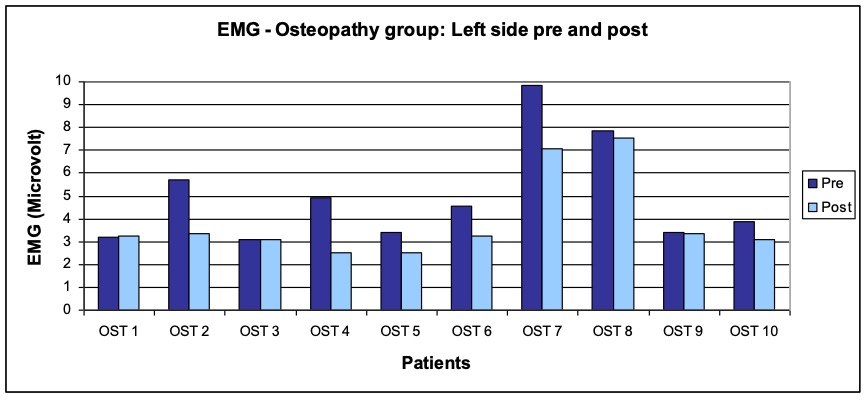
Figure 41: EMG – OST group: Left side pre and post
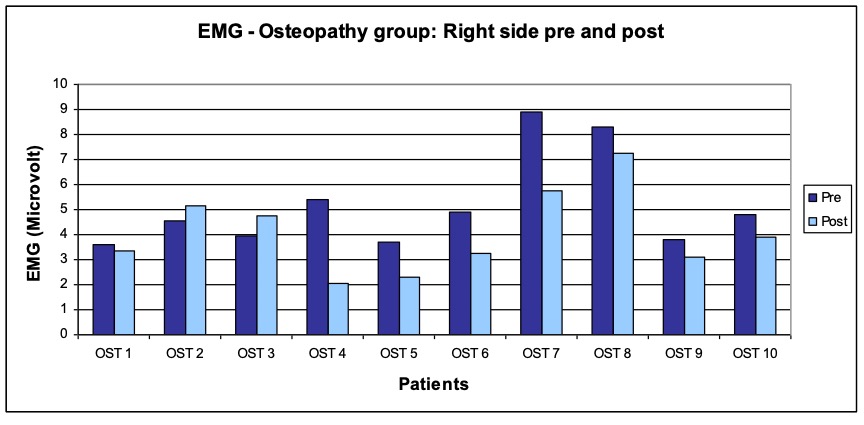
Figure 42: EMG – OST group: Right side pre and post
Before the treatments the mean value (pre) of the MT group for the EMG measurements was 4.58 (left) and 4.99 (right). Through the treatments a mean improvement (reduction) of -0.57 and thus a mean value (post) of 4.42 could be achieved for the right side, which was with p=0.018 a significant improvement for the MT group. A deterioration (increase) of 0.77 and thus a mean value (post) of 5.35 could be observed on the left side for the MT group, a result which, however, was with p=0,229 statistically not significant (cf. Table 23).
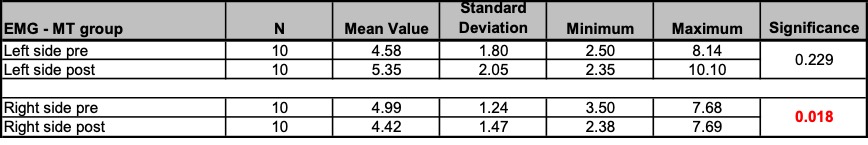
Table 23: EMG – MT group: Results; Unit of measurement: Microvolt
Figure 43 illustrates the pre and post EMG values on the left side for all patients in the MT group, while Figure 44 represents the same for the right side. On the right side almost all patients showed an improvement after the treatment (with the exception of MT 1, MT 3 and MT 7). On the left side, however, the values deteriorated for more than half of the patients.
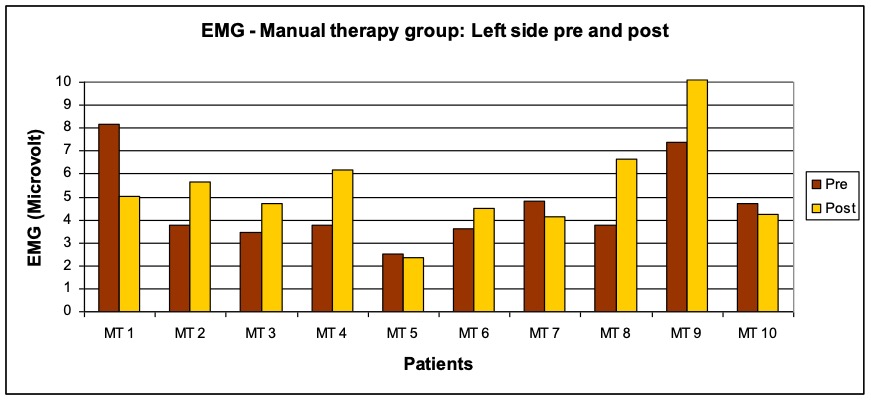
Figure 43: EMG – MT group: Left side pre and post
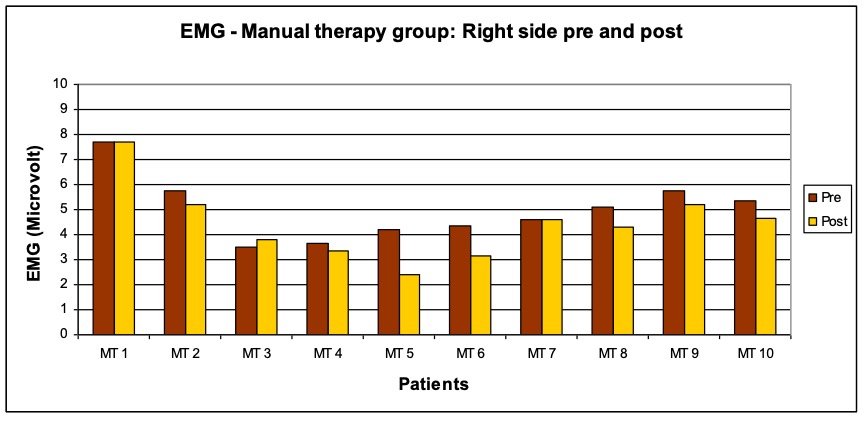
Figure 44: EMG – MT group: Right side pre and post
Figure 45 provides a graphic comparison of the pre and post EMG values on the left and right side for all patients, for the OST group and for the MT group in a boxplot diagram.
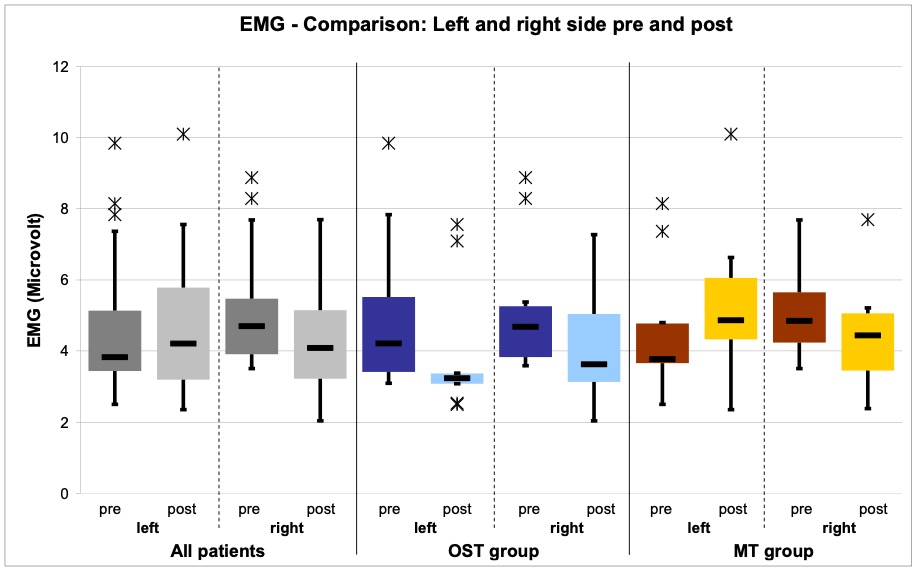
Figure 45: EMG – Comparison: Left and right side pre and post
For the OST group a mean improvement of -1.08 on the left and -1.10 on the right side could be achieved. In the MT group, however, only the right side improved by
-0.57, while on the left side a deterioration of 0.77 occurred.
In comparison with p=0,015 osteopathy was significantly more effective than manual therapy (according to the CRAFTA® concept) on the left side, which is due to the fact that the MT group got worse on this side. On the right side no difference regarding the effectiveness of the two treatment forms could be observed. Further details can be gathered from Table 24.
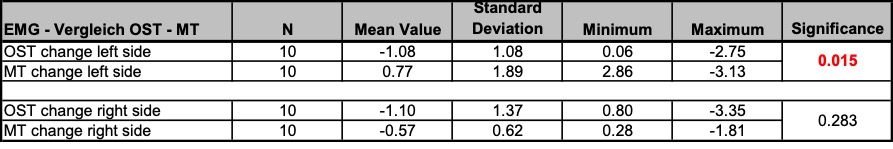
Table 24: EMG – Comparison OST – MT; Unit of measurement: Microvolt
Figure 46 provides a graphic comparison of the changes in the EMG values on the left and right side for all patients, for the OST group and for the MT group in a boxplot diagram. A reduction (negative value) corresponds to an improvement.
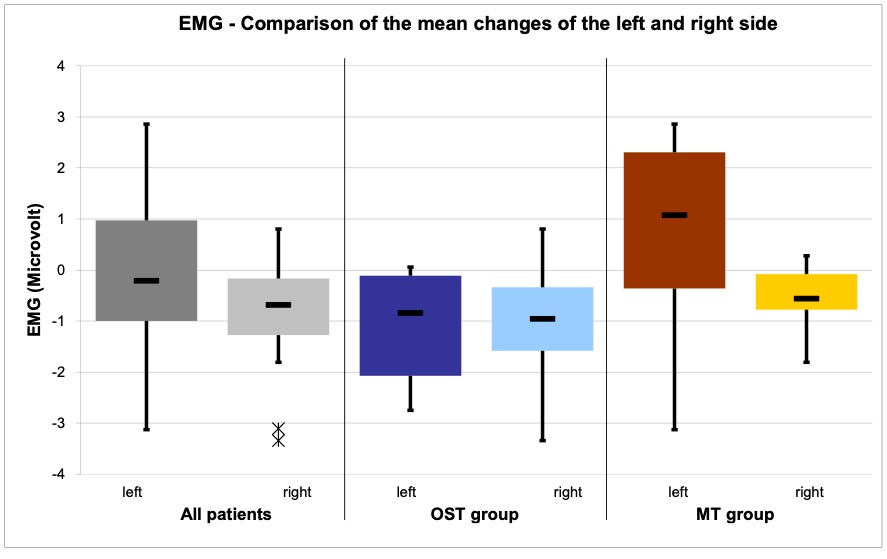
Figure 46: EMG – Comparison OST – MT
Discussion and conclusions
The objective of this clinical pilot study was to compare osteopathy with manual therapy (according to the CRAFTA® concept) with regard to their effectiveness for the treatment of patients with CMD. At a first glance, the hypothesis that osteopathy would show better results can be confirmed on the basis and within the framework of this study.
Table 25 provides a summary of the most important results that were presented in the previous Chapter 4.
Table 25: Summary of the results
Considering all patients, the treatments achieved for almost all of the 9 categories of the 4 measurement parameters highly significant improvements. Only the improvement of the health concept role physical of the SF36 questionnaire was (marginally) not significant. Furthermore, the EMG measurement on the left side did not show positive results due to a (not significant) deterioration of the MT group (in contrast to a significant improvement of the OST group).
For the OST group the significance of the improvements was even more pronounced than that for all the patients as a collectivity. It could be observed that osteopathy achieved significant improvements in 8 of the 9 categories. Moreover, a direct comparison showed that osteopathy was also in 5 of these categories significantly more effective than manual therapy (according to the CRAFTA® concept).
In contrast, the manual therapy (according to the CRAFTA® concept) achieved only in 3 of the 9 categories significant improvements and the comparison showed that it was in none of the categories more effective than osteopathy.
In the following the results of the various measurement methods for the 4 measurement parameters (cf. Chapters 5.1 to 5.4) are discussed and compared with available results from the literature. Among the mentioned studies (cf. Chapter 1) only the study by Knust (2006) and to a limited extent the study by Demling et al. (2008) are suitable for a comparison due to their study design and their choice of measurement parameters and methods. Further, the design and the implementation of the present study is critically evaluated (cf. Chapter 5.5). Finally, a conclusion is drawn on the basis of the discussed results (cf. Chapter 5.6).
Pain, VAS assessment and SES (pain perception) questionnaire
In the VAS assessment (pain intensity) the osteopathic treatments could achieve a significant improvement for the patients of the OST group. In addition, a direct comparison with the MT group, which was treated with manual therapy (according to the CRAFTA® concept), showed that osteopathy was significantly more effective.
However, when the VAS results of the MT group are considered in more detail, it can be recognized that the average improvement with p=0.057 was only marginally not significant. 2 of the 10 patients of the MT group (MT 1 and MT 9) indicated a pain intensity of 0 before and after the treatments, i.e. they did not suffer from any pain at these moments at all. In the OST group, on the other hand, all patients indicated a pain intensity of at least 2 points before the treatments.
Nevertheless, the statistical analysis showed that the starting conditions were similar for both groups, even though the average “initial pain level” of the MT group (3.60) was almost one point lower than that of the OST group (4.53). Further details regarding the results can be found in Chapter 4.1.
Also regarding the SES questionnaire (pain perception) the osteopathic treatments could achieve significant improvements in both categories, the global dimension affective and the global dimension sensory. In comparison with the manual therapy (according to the CRAFTA® concept) osteopathy showed a significantly better effectiveness in the global dimension sensory, although the manual therapy (according to the CRAFTA® concept) also could achieve a significant improvement in this category.
A closer look at the other global dimension (affective) reveals that here (like in the VAS assessment) the improvement of the MT group was with p=0.055 only marginally not significant. In the case of the SES questionnaire the “initial pain level” was slightly lower of the MT group (global affective = 20.60 and global sensory = 13.10) than that of the OST group (global affective = 24.50 und global sensory = 16.60) – just like it was the case in the VAS assessment. The statistical analysis of the SES starting conditions for both groups showed that the values of the traits Persistency and Local Intrusion were significantly higher in the OST group than in the MT group. After the treatments, however, no significant differences could be observed for the two groups. Further details regarding the results can be found in Chapter 4.2.
Considering the results of the pilot study by Knust (2006) where a significant pain reduction due to manual therapy (including the application of some CRAFTA® techniques in the craniomandibular region) could be achieved and considering the small number of participants in the present study with only marginally not significant results (VAS and SES global dimension affective) for the MT group, it can be concluded that the manual therapy (according to the CRAFTA ® concept) normally should be able to achieve significant improvements regarding the treatment of pain in patients with CMD. However, the results of the present study showed that the effectiveness of osteopathy was significantly better in this respect.
Quality of life, SF36 questionnaire
Regarding the parameter (health-related) quality of life, which was determined through the SF36 questionnaire in this study, osteopathic treatments could achieve highly significant improvements of the mental summary scale and of the category change in health. In addition, osteopathy was significantly more effective in these categories than manual therapy (according to the CRAFTA® concept). With regard to the physical summary scale, osteopathy was with p=0.05 marginally not significantly better than manual therapy (according to the CRAFTA® concept). For the MT group no significant improvement in any of the categories of the measurement parameter quality of life could be observed. On the contrary, it was striking that actually a (not significant) deterioration of the mental summary scale was recognized and that the category change in health remained the same. Further details regarding the results can be found in Chapter 4.3.
The SF36 questionnaire was chosen and used on purpose. The aspect of the health-related quality of life should allow for a better holistic consideration of the patient’s condition and thus leave more scope for the assessment in particular regarding the effectiveness of the osteopathic treatment. The SF36 questionnaire is a measuring instrument that is widely used and recognized on an international level (cf. Bullinger et al. 1998) and was already used in other osteopathic works, e.g. by Recknagel et al. (2004) and Kiessling et al. (2004) at the Akademie für Osteopathie (AFO) as well as by Hölscher et al. (2007) at the Hogeschool Zuyd in Heerlen.
The results of this study indicate that the use of a “holistic measurement parameter” in form of the health-related quality of life absolutely made sense. The initial, implied assumption that the two treatment methods will differ in this context was confirmed. Osteopathy could achieve significant improvements of this holistic measurement parameter, in particular in comparison with the manual therapy (according to the CRAFTA® concept). This success among others can be attributed to the holistic treatment approach of osteopathy, which clearly differentiates osteopathy from manual therapy.
Mouth opening, IID measurement
Regarding the objectively measurable parameter mouth opening both, osteopathy and manual therapy (according to the CRAFTA® concept), could achieve highly significant successes. A direct comparison of the two treatment methods did not reveal any differences. Further details regarding the results can be found in
Chapter 4.4.
The results for the MT group in this study correspond to those of the pilot studies by Knust (2006) and Demling et al. (2008), who also observed a significant improvement of the mouth opening through manual therapy. All patients in this study ranged after the treatments above the “scientific threshold” of 40 to 42 mm (cf. Bumann et al. 2000, Stelzenmüller et al. 2004).
Muscle tension, Biofeedback EMG measurement
Like the mouth opening, the muscle tension is an objectively measurable parameter. The osteopathic treatments could achieve significant improvements for the EMG measurements on the right and left side. On the left side osteopathy was also significantly more effective than the manual therapy (according to the CRAFTA® concept), which only obtained significant improvements on the right side. On the left side actually a (not significant) deterioration could be observed for the MT group. Further details regarding the results can be found in Chapter 4.5.
Considering the patients and the distribution of their problems between the left and right side of the face, it can be recognized that the majority of the problems (pain, deviation, clicking) occurred on the left side. 16 of the 20 patients indicated problems on the left side and only 10 problems on the right side. The distribution among the two groups showed an even greater imbalance. Among the 10 patients of the MT group 9 indicated problems on the left side and only 4 on the right side. In contrast, the OST group was almost balanced with 7 of the 10 patients indicating problems on the left side and 6 on the right side. This distribution can explain the bad EMG result of the MT group on the left side.
Since manual therapy (according to the CRAFTA® concept) often applies techniques directly at the site of the complaints, these treatments may have caused a higher reactive muscle tension on the left side in the M. masseter. Despite a period of rest of about 5 minutes after the last treatments, the final EMG measurements (post) on average showed higher values on the left side than the initial EMG measurement before the treatments (pre).
If the period of rest before the final EMG measurement would be extended or the measurement would be carried out at a later appointment (only control), this bad result and thus probably the significantly better results of the osteopathic treatments may be put into perspective. Even though osteopathy also uses techniques directly at the site of the complaints, in this case at the TMJ, the techniques are applied less frequently and with a lesser degree of intensity than the techniques used by the manual therapy (according to the CRAFTA® concept) because osteopathy follows a holistic approach and intends to integrate and balance structures.
Design and implementation of the study
A retrospective critical consideration of the design and implementation of this clinical pilot study highlights the following aspects:
Although the age and gender distribution of the participants do not offer any points of criticism since the age curve of the patients and the disproportionate high share of women in this study are typical for CMD (cf. Ahlers et al. 2007). Only the small number of participants can be regarded as a weakness.
The treatments were delivered by two different therapists. They were neither made anonymous nor was there an alternation of the therapist. Even though both therapists have significant experiences in the treatment of CMD, a general difference in the quality of treatments and the therapists’ skills cannot be excluded, in particular since the author of the study, who treated the OST group, is not only an osteopath but also a certified CRAFTA® therapist. In addition, differences in gender and sympathy of the therapists may have had a subconscious influence on the patients. The presence of a neutral, passive observer and the treatment of the different groups by several alternating (calibrated) therapists might eliminate this weakness.
Regarding the number and duration of the treatments as well as the study period, it would make sense to add another final check-up appointment (e.g. without any treatment but only for final measurements and questioning) to be able to better differentiate between short-term effects and long-term improvements.
The selected measurement parameters and methods have in general proven to be reasonable and manageable, in particular the SF36 questionnaire to establish the health-related quality of life as “holistic measurement parameter“. However, each patient in this study had to complete two (extensive) questionnaires at the beginning and at the end of the course of treatments. Maybe the study could have done without the SES questionnaire. In addition, it has to be pointed out that the EMG measurements with the biofeedback device were quite elaborate and expensive since the device could only be used for this study. Nevertheless, the EMG measurement can in principle be recommended as an objective measurement method, in particular for a regular verification of the success of the treatments and for the documentation of each patient (cf. Hülse et al. 2003).
On the basis of the results discussed in the previous chapters the following conclusions can be drawn from this clinical pilot study:
Regarding the measurement parameters pain, mouth opening and muscle tension both, osteopathy and manual therapy (according to the CRAFTA® concept) facilitate significant improvements for the treatment of patients with CMD. In this context osteopathy is significantly more effective concerning the parameter pain. Regarding the health-related quality of life only osteopathy has a significant effect and in comparison works significantly better than manual therapy (according to the CRAFTA® concept) which could not achieve an improvement of this parameter at all.
A follow-up study over a longer period of time (with an additional final check-up appointment) and with more participants, who are treated alternately by a team of therapists is recommended to verify the results of the present study and to put them on a sound basis., die durch ein Therapeutenteam behandelt werden, sei an dieser Stelle empfohlen, um die Ergebnisse dieser Arbeit zu überprüfen und auf eine sichere Basis zu stellen.
| A. | artery |
| AAOP | American Academy of Orofacial Pain |
| AFO | Academy of Osteopathy |
| Art. | Articulatio / Joint |
| cf. | confer |
| CMD | craniomandibular dysfunctions |
| CRAFTA® | Cranial Facial Therapy Academy |
| DGFDT | German Society for function diagnostics and therapy |
| DGZMK | German Society for dental, oral and craniomandibular therapies |
| EMG | electromyography |
| ENT | Ear Nose Throat |
| et al. | and others |
| IHS | International Headache Society |
| Lig. | ligament |
| M. | Musculus |
| MPI | Mandibula-Positions-Indikator |
| MT | Manual therapy |
| MRT | magnetic resonance tomography |
| N. | nerve |
| Ncl. | nucleus |
| OST | Osteopathy |
| RCT | Randomized Controlled Trial |
| RDC | Research Diagnostic Criteria |
| SES | pain perception scale |
| IID | inter-incisor distance |
| TMD | Temporomandibular Disorders |
| TMJ | Temporomandibular joint |
| UPPM | Upright Postural Position of the Mandible |
| V. | vein |
| VAS | Visual analogue scales |
| vs. | Versus |
7.1 Abbildungsverzeichnis
Figure 1: Conceptual framework of the thesis 6
Figure 2: Model of the TMJ integration in the vertical body statics 11
Figure 3: The primary jaw joint is replaced by the Articulatio
Temporomandibularis as a secondary jaw joint 13
Figure 4: Overview “Patient with cranio-fascial dysfunctions and pain” 17
Figure 5: Symptoms of a CMD 22
Figure 6: Interrelations of TMJ and body via myofascial chains 29
Figure 7: Visual Analogue Scale by the company Painscale 39
Figure 8: IID measurement with a ruler 45
Figure 9: EMG module of the Biofeedback device 2000 x-pert
by the company Schufried and one-way adhesive electrode
Blue Sensor M by the company Ambu 47
Figure 10: Determination, measurement and documentation of the coordinates
for the surface electrodes of the EMG measurement 49
Figure 11: Example of an EMG measurement with the biofeedback device
2000 x-pert by the company Schufried 51
Figure 12: Example of a comparison of the first and second EMG measurement
with the biofeedback device 2000 x-pert by the company Schufried 51
Figure 13: Distribution of the patients 53
Figure 14: Age distribution: All patients 53
Figure 15: Age distribution: OST group 54
Figure 16: Age distribution: MT group 54
Figure 17: Gender distribution: All patients 55
Figure 18: Inclusion criteria: All patients 55
Figure 19: Inclusion criteria: OST group 56
Figure 20: Inclusion criteria: MT group 56
Figure 21: VAS – OST group pre and post 57
Figure 22: VAS – MT group pre and post 58
Figure 23: VAS – Comparison pre and post 59
Figure 24: VAS – Comparison OST – MT 60
Figure 25: SES – Global dimensions: OST group pre and post 62
Figure 26: SES – Traits: OST group pre and post 63
Figure 27: SES – Global dimensions: MT group pre and post 64
Figure 28: SES – Traits MT group pre and post 65
Figure 29: SES – Comparison global dimensions pre and post 66
Figure 30: SES – Comparison OST – MT 67
Figure 31: SF36 – Summaries: OST group pre and post 70
Figure 32: SF36 – Health concepts: OST group pre and post 70
Figure 33: SF36 – Summaries: MT group pre and post 72
Figure 34: SF36 – Health concepts: MT group pre and post 72
Figure 35: SF36 – Comparison: Summaries pre and post 73
Figure 36: SF36 – Comparison OST – MT 75
Figure 37: IID – OST group pre and post 76
Figure 38: IID – MT group pre and post 77
Figure 39: IID – comparison pre and post 78
Figure 40: IID – Comparison OST – MT 79
Figure 41: EMG – OST group: Left side pre and post 81
Figure 42: EMG – OST group: Right side pre and post 81
Figure 43: EMG – MT group: Left side pre and post 82
Figure 44: EMG – MT group: Right side pre and post 82
Figure 45: EMG – Comparison: Left and right side pre and post 83
Figure 46: EMG – Comparison OST – MT 84
List of tables
Table 1: Research Diagnostic Criteria for Temporomandibular
Disorders (RDC/TMD), 25
Table 2: Comparison of osteopathy with manual therapy (CRAFTA ® concept)
for the treatment of patients with CMD 30
Table 3: Overview of items, traits and global dimensions of the SES 40
Table 4: Overview and description of the summary scales and health concepts
of the SF36 questionnaire 43
Table 5: VAS – All patients: Results 57
Table 6: VAS – OST group: Results 57
Table 7: VAS – MT group: Results 58
Table 8: VAS – Comparison OST – MT 59
Table 9: SES – All patients: Results 61
Table 10: SES – OST group: Results 62
Table 11: SES – MT group: Results 64
Table 12: SES – Comparison OST – MT 67
Table 13: SF36 – All patients: Results 68
Table 14: SF36 – OST group: Results 69
Table 15: SF36 – MT group: Results 71
Table 16: SF36 – Comparison: OST – MT 74
Table 17: IID – All patients: Results 76
Table 18: IID – OST group: Results 76
Table 19: IID – MT group: Results 77
Table 20: IID – Comparison OST – MT 78
Table 21: EMG – All patients: Results 80
Table 22: EMG – OST group: Results 80
Table 23: EMG – MT group: Results 82
Table 24: EMG – Comparison OST – MT 83
Table 25: Summary of the results 85
AHLERS, M. O.; JAKSTAT, H. A. (2007):
Klinische Funktionsanalyse – Interdisziplinäres Vorgehen mit optimierten Dokumentationshilfen, 3. Auflage, Hamburg: denta Concept Verlag.
AMIGUES, J.-P. (2005):
Das stomatognathe System aus osteopathischer Sicht, DO, 3, 12-15.
BREUL, R. (2005):
Das Kiefergelenk des Menschen, DO, 3, 16-21.
BUMANN, A., LOTZMANN, U, (2000):
Funktionsdiagnostik und Therapieprinzipien. Stuttgart: Georg Thieme Verlag.
BUTENSCHÖN, W.; MITHA, N. (2002):
Einfluss osteopathischer Behandlung auf craniomandibuläre Dysfunktionen,
Hamburg: DO-Arbeit, SKOM.
BULLINGER, M.; KIRCHBERGER, I. (1998):
SF36 Fragebogen zum Gesundheitszustand, Handanweisung,
Göttingen: Hogrefe Verlag.
CLARK, G. T., BROWNE, P.A., NAKANO, M., YANG, Q. (1993):
Coactivation of sternocleidomastoid muscles during maximum clenching.
Journal of Dental Research 72, 1499-1502.
COSTEN, J.B. (1934):
Syndrome of ear and sinus symptoms dependent upon disturbed
function of the temporomandibular joint. Am. Otol. Rhin., 43, 1-15.
CROIBIER, A. (2006):
Diagnostik in der Osteopathie, München: Urban & Fischer Verlag.
DAHL, H. ; RÖßLER, A. (1999):
Grundlagen der Manuellen Therapie, Stuttgart: Georg Thieme Verlag.
DAPPRICH, J. (2007):
Vorbehandlung und Therapie der craniomandibulären Dysfunktion. Zahnheilkunde, Management ,Kultur, 23, 306-313.
DE KNATER, R., TRUIN, G., BURGERSDIJK, R., KALSBEEK, H., et al.(1993):
Prevalence in the Dutch adult population a meta – analysis of signs and symptoms of temporomandibular disorder. Journal of Dental Research, 72, 1509-1518.
DEMLING, A., ISMAIL, F., HEßLING, K., FINK, M., STIESCH_SCHOLZ, M. (2008):
Pilostudie zum Einfluss von physikalischer Therapie auf objektive und subjektive Parameter bei CMD. Deutsche Zahnärztliche Zeitschrift, 63, 3, 190-200.
DIMITROULIS, G., GREMILLION, H., DOLWICK, F., WALTER, J. (1995):
Temporomandibular disorders. Non-surgical treatment. Australian Dental Journal, 40, 6, 372-376.
DITTEL, R. (1992):
Schmerzphysiotherapie, Lehr- und Handbuch des Neuromedizinkonzepts.
Stuttgart: Gustav Fischer Verlag.
DWORKIN, S.F., LE RESCHE, L. (1992):
Research diagnostic criteria for temporomandibular disorders: Review, criteria,
examinations and specifications, critique.
Journal of Craniomandibular Disorders, 6, 301-355.
ETTLIN, M. E.; KAESER, H. E. (1998):
Muskelverspannungen, Ätiologie, Diagnostik und Therapie,
Stuttgart: Georg Thieme Verlag.
FINK, M.G. (2000):
Physikalische Medizin bei schmerzhaften Erkrankungen der Kiefergelenksregion,
zahnmedizin-online, 10, 74.
FRYMANN, V. M. (1983):
Cranial Osteopathy and its Role in Disorders of the TMJ,
Dental Clinics of North America, 27, 595 – 611.
GEISSNER, E. (1996):
Die Schmerzempfindungs-Skala, Handanweisung. Göttingen: Hogrefe Verlag.
GERNET W., RAMMELSBERG P. (2000):
Kiefergelenkerkrankungen und Funktionsstörungen. In: SCHWENZER, N., EHRENFELD, M. (Hrsg.), Zahnärztliche Chirurgie, Band 3, 3. Auflage,
Stuttgart: Georg Thieme Verlag, 263-265.
GESCH, D. BERNHARDT, O., MACK, F. (2004):
Okklusion und subjektive Kiefersymptome bei Männern und Frauen. Ergebnisse der Study of Health in Pomerania (SHIP).
Schweizer Monatsschrift für Zahnmedizin, 114, 573-580.
GLEDITSCH; J.M. (2004):
Akupunktur in der Therapie der craniomandibulären Thrapie. In: SCHÖTTL, R., LOSERT-BRUGGNER, (Hrsg.), ICCMO Kompendium, Rastatt: Geiserdruck.
GOHL-FROHNMAYER, P. (2005):
Störungen in der Entwicklung des kindlichen Kiefers. DO, 3, 7-11.
GRANDJEAN, M.; BORNHOFEN, P. (2003):
Warum denn so verbissen? Kiefergelenkstörungen – eine neue Volkskrankheit aus ganzheitlicher Sicht. Sulzberg: Joy Verlag.
GÜNDEL; H., NEFF, A. (2006):
Anhaltender idiopathischer Gesichtsschmerz bzw. craniomandibulare Dysfunktion. In: HENNINGSEN, P., GÜNDEL, H., CEBALLOS-BAUMANN, A. (Hrsg.) Neuro-Psychosomatik, Grundlagen und Klinik neurologischer Psychosomatik,
Stuttgart: Schattauer Verlag.
HIPPEL, S. (2006):
Das Kiefergelenk – zahnärztliche und osteopathische Methoden im interdisziplinären Austausch, Schlangenbad: DO-Arbeit, College Sutherland.
HONIKEL, M. (2007):
Das Craniomandibuläre System Teil 1, Osteopathische Medizin, 2, 22 – 26.
HONIKEL, M. (2007):
Das craniomandibuläre System und seine Effekte auf die Körperhaltung Teil 2,
Osteopathische Medizin, 3, 16 – 21.
HONIKEL, M. (2007):
Das craniomandibuläre System und seine Effekte auf die Körperhaltung Teil 3
Osteopathische Medizin, 4, 4 – 9.
HÖLSCHER, M., NOTARIUS, R. (2007):
Effektivität der osteopathischen Behandlung von Patienten mit chronischer Achilles – Tendinopathie. Heerlen: Bachelor Abschlußarbeit, Hogeschool Zuyd.
HUELSE, M.; LOSERT-BRUGGNER, B. (2003):
Die Bedeutung elektromyographischer Messungen in der Diagnostik und Therapie von craniomandibulären Dysfunktionen,
Zeitschrift für Physiotherapeuten, 55, 230 – 235.
JOHANNSEN, M. (2008)
Vortrag: „Was ist eigentlich eine klinische Studie?“ Charitè Berlin
www.lh-nierenkrebs.org/d/3312 [11.10.2008]
KARES, H., SCHINDLER, H., SCHÖTTL, R. (2001):
Der etwas andere Kopf- und Gesichtsschmerz, Craniomandibuläre Dysfunktion – CMD, Rastatt: Greiserdruck – Verlag.
KEHR, O. (2005):
Einfluss der Magnesiumsubstitution auf das Beschwerdebild der Craniomandibulären Dysfunktion (CMD), Graz / Schloss Seggau: Master Thesis, Interuniversitäres Kolleg für Gesundheit und Entwicklung.
KERSCHBAUM, T., LIEBRECHT, S., MENTLER-KÖSER, M. (2001):
Klinische Erfahrungen mit Physiotherapie bei Patienten mit schmerzhaften Funktionsstörungen. Deutsche Zahnärztliche Zeitschrift, 56, 9, 523-526.
KIESSLING, G., TRANTENROTH, M. (2004):
The osteopathic treatment of patients with coxarthritis. DO-Arbeit, Akademie für Osteopathie.
KLUCKHUHN, C. (2006):
Wenn die Seele knirscht. zm-online, 96, 4, 32-36.
KNUST, M. (2006):
Die Behandlung der kraniomandibulären Dysfunktion – eine randomisierte Pilotstudie
zur manuellen Therapie versus Übungsbehandlung, Osnabrück: Bachelorarbeit,
Fachhochschule Osnabrück.
KOOL, J.; DE BIE, R (2001):
Der Weg zum wissenschaftlichen Arbeiten, Stuttgart: Georg Thieme Verlag.
KÖNEKE, C. (2005):
Die interdisziplinäre Therapie der Craniomandibulären Dysfunktion,
Berlin: Quintessenz Verlag.
KONRAD, P. (2005):
EMG-Fibel, Eine praxisorientierte Einführung in die kinesiologische Elektro
myographie, Version 1.0, Noraxon INC. USA, www.velamed.com
KOPP, S.; PLATO, G.; SEBALD, W. G. (2000):
Kraniomandibuläre Dysfunktion – Eine Standortbestimmung,
Manuelle Medizin, 38, 335 – 341.
KORN, H. – J. (2005):
Biofeedback und zahnmedizinische Behandlungsansätze bei temporomandibulären Störungen und Bruxismus, Verhaltenstherapie, 15, 94 – 102.
LE RESCHE, L., MANCL, L., SHERMAN, JJ. (2003)
Changes in temporomandibular pain and other symptoms across the menstrual cycle. Pain: 106, 253-261.
LANG, J (2001):
Skull Base and Related Structures, Atlas of Clinical Anatomy.
Stuttgart: Schattauer Verlag.
LIEM, T. (2000):
Praxis der kraniosakralen Osteopathie, Stuttgart: Hippokrates Verlag.
MADSEN, H. (2005):
Myoarthropathien des Kausystems und orthopädische Befunde – ein klinisch relevanter Zusammenhang? Kieferorthopädie, 19, 183-192.
MAGOUN, H. (1975):
Dental equilibration and osteopathy, JAOA, 74, 981 – 991.
MAGOUN, H. (1974):
The temporal bone – Troubelmaker in the Head, JAOA, 73, 825 – 835.
MC NEILL, C. (1990):
Craniomandibular disorders. Guidelines for evaluation, diagnosis and management.
Chicago: Quintessenz Verlag
MENSE, S. (1998):
Pathophysiologie der Muskelverspannungen. In: ETTLIN, M. E.; KAESER, H. E. (Hrsg.): Muskelverspannungen, Ätiologie, Diagnostik und Therapie,
Stuttgart: Georg Thieme Verlag.
MILNE, H. (1999):
Aus der Mitte des Herzens lauschen, Band 2, Petersberg: Via Nova Verlag.
NEUHUBER, W.L. (2004):
Die Nacken-Kiefer-Balance. In: SCHÖTTL, R.; LOSERT-BRUGGNER, B. (Hrsg.): ICCMO-Kompendium, Rastatt: Greiserdruck – Verlag.
NICOLAKIS, P., ERDOGMUS, B., KOPF, A. EBENBICHLER, G., et al. (2001):
Effectiveness of exercise therapy in patients with internal derangement of the temporomandibular joint, Journal of Oral Rehabilitation, 28, 1158-1164.
O´RAHILLY, R., MÜLLER, F. (1999):
Embryologie und Teratologie des Menschen, Bern: Hans Huber Verlag.
PLATO, G. (2001):
Gesichtsschmerz aus manualmedizinischer und kieferorthopädischer Sicht
Manuelle Medizin, 39, 254-258.
RAUBER, A.; KOPSCH, F. (1987):
Anatomie des Menschen, Bewegungsapparat, Stuttgart: Georg Thieme Verlag.
RECKNAGEL, A., Koop, C. (2004):
The Influence of Osteopathic Treatment at chronic Vertigo. DO-Arbeit, Akademie für Osteopathie.
ROCABADO, M. (1983):
Biomechanical Relationship of the Cranial, Cervical and Hyoid Regions,
The Journal of craniomandibular Practice, 3, 62 – 65.
ROSENOW, D., TRONNIER, V., GÖBEL, H. (2004):
Neurogener Schmerz, Berlin: Springer Verlag.
SADER, R. (2005):
Ein erster Schritt: Neuartiges künstliches Kiefergelenk zum ersten Mal in Frankfurt eingesetzt, www.innovationsreport.de.
SADLER, T.W. (1998):
Medizinische Embryologie, Stuttgart: Georg Thieme Verlag.
SANDERS, B. (1988):
Chirurgische Behandlung der fortgeschrittenen inneren Verlagerung und Arthrose des Kiefergelenks. In: CLARK, G. T.; SOLBERG, W. K (Hrsg.) Perspektiven der Kiefergelenksstörungen, Berlin: Quintessenz Verlag.
SCHERFER, E. (2005):
Evidenz für die Wirksamkeit von Behandlungsmethoden und –protokollen – aber auf welchem Niveau?, Zeitschrift für Physiotherapeuten, 57, 1578 – 1584.
SCHUHFRIED, G. (2006):
Biofeedback 2000 x-pert, Bedienungsanleitung, Mödling.
SCHUPP, W. (2005):
Kraniomandibuläre Dysfunktionen und deren periphere Folgen – Eine Lieteraturübersicht, Manuelle Medizin, 43, 29-33.
SIEBER, M., GRUBENMANN, E., RUGGIA, G.M., PALLA, S., (2003):
Relation between stress and symptoms of craniomandibular disorders in adolescents. Schweizer Monatsschrift für Zahnmedizin 113, 648-654.
SIEBERT, G. (2000):
Atlas der zahnärztlichen Funktionsdiagnostik. München: Hanser Verlag.
SLAVICEK, G., GSELLMANN, B.; GRUBER, R.; RATH, M.; FURHAUSER, R. (1995)
Biofeedback als Therapieergänzung bei craniomandibularer Dysfunktion,
IOK-Informationen aus Orthodontie & Kieferorthopädie, Jhrg. 27, Nr. 1.
SLAVICEK, G. (2004):
Craiomandibuläre Funktionsstörungen in der täglichen Praxis. Thüringer Zahnärzteblatt, 06, 23-26.
STELZENMÜLLER, W.; WIESNER, J. (2004):
Therapie von Kiefergelenkschmerzen – Ein Behandlungskonzept für Zahnärzte, Kieferorthopäden und Physiotherapeuten, Stuttgart: Georg Thieme Verlag.
STIBENZ, C. (2004):
Klinische Assessments craniomandibulärer Dysfunktionen (CMD)
Jena: Dissertation, Friedrich Schiller Universität.
STILL; A.T. (1899):
The Philosophy of Osteopathy, Reprint 2006, Pähl: Jolandos – Verlag.
TÜRP, J.C. (2002):
Orofacialer Schmerz, Schmerz, 16, 337-338.
UMSTADT, H.E. (2002):
Botulinumtoxin in der MKG-Chirurgie. Mund Kiefer Gesichts Chirurgie 6, 249-260
VAN ASSCHE, R. (2006):
The Influence of the Tonus of the Suboccipital Muscular System on the Tonus of the Masseter and the Sympathetic Nervous System, Wien/Krems: Master Thesis, Donauuniversität Krems.
VAN DEN BERG, F., WOLF, U. (2002):
Manuelle Therapie. Sichere und effektive Manipulationstechniken.
Heidelberg: Springer-Verlag.
VERVERS, M., OUWERKERK, J., VAN DER HEIJDEN, G., STEENKS, M. (2004):
Ätiologie der kraniomandibulären Dysfunktion: eine Literaturübersicht
Deutsche Zahnärztliche Zeitschrift, 59, 556-562.
VON HEYMANN, W. (2007):
Orthopädie und craniomandibuläre Dysfunktion. In: KÖNEKE, C. (Hrsg.) 8. Bremer CMD-Symposium, Waabs: GCA-Verlag.
VON LINDERN, J., NIEDERHAGEN, B., APPEL, T., BERGÉ, S. REICH, R. (2000):
Die Behandlung muskulärer Hyperaktivität der Kaumuskulatur mit Botulinumtoxin
Typ A, Deutsche Zahnärztliche Zeitung, 55, 26-29.
VON PIEKARTZ, H. J. M. (2005):
Kiefer, Gesichts- und Zervikalregion – Neuromuskuloskeletale Untersuchung, Therapie und Management, Stuttgart: Georg Thieme Verlag.
VON PIEKARTZ, H. J. M. (2007):
Effektivität von neuromuskuloskeletaler Behandlung (CRAFTA®) von Patienten mit chronischen kraniomandibulären- facialen Dysfunktionen und Schmerzen. Eine Pilotstudie, Hamburg: CRAFTA® Kongress-Unterlagen.
VON TREUENFELS, H. (1984):
Kopfhaltung, Atlasposition und Atemfunktion beim offenen Biss. Fortschritte der Kieferorthopädie, 45, 111-121.
WICKER KLINIK BAD HOMBURG (2008):
Schmerzzustände. http://www.schmerz-zustaende.de [11.10.2008]